When you take a pill, your body doesn’t just absorb it and call it a day. It has to break it down—mostly in the liver—and that’s where CYP3A4 inhibition, a process where certain substances block a key liver enzyme that breaks down drugs. Also known as CYP3A4 enzyme suppression, it can turn a safe dose into an overdose, or make a drug useless. This isn’t some rare lab phenomenon. It’s happening right now to people taking common meds like statins, blood pressure pills, or even anti-anxiety drugs.
Think of CYP3A4 as a gatekeeper. It’s one of the most important enzymes in your liver, responsible for processing over half of all prescription drugs. When something like grapefruit juice, certain antibiotics, or even St. John’s wort steps in and blocks it, your body can’t clear the drug fast enough. That means levels build up. Suddenly, a normal dose of a cholesterol med turns into a risk for muscle damage. A sleep aid becomes too strong. A painkiller starts affecting your heart. This is why drug interactions, when one substance changes how another works in your body aren’t just warnings on a label—they’re real, measurable dangers. And it’s not just pills. Supplements like kava or herbal teas can do the same thing, as shown in posts about kava and sedatives or herbal remedies for sore throats. Even foods like grapefruit, garlic, or leafy greens can throw off your meds, as covered in multiple articles here.
What makes this even trickier is that CYP3A4 inhibition doesn’t always show up right away. You might take your meds for months without issues—then add a new supplement, or switch to a different brand of grapefruit juice, and suddenly feel dizzy, nauseous, or weak. That’s not just bad luck. That’s your enzyme system being overwhelmed. It’s why drug take-back programs exist—not just to keep meds out of water supplies, but because unsafe combinations can be deadly. And it’s why knowing your meds’ metabolism matters more than you think. If you’re on anything for heart disease, depression, pain, or even erectile dysfunction, CYP3A4 is likely involved. The same enzyme that breaks down your blood pressure pill also handles the generic version of Viagra, the anti-inflammatory you take for arthritis, and the antibiotic your doctor prescribed last winter.
You don’t need to memorize biochemistry to stay safe. But you do need to ask the right questions. What else are you taking? Is that new supplement really safe? Could that citrus fruit be messing with your pills? The posts below break down real cases—like how erythromycin or ketoconazole can shut down CYP3A4, how hydroquinone and retinoids interact with liver metabolism, and why mixing Toradol with other NSAIDs can be risky beyond just stomach upset. You’ll see how common drugs like Ceclor, Flonase, and even Nurofen can be affected. This isn’t theory. It’s what’s happening in people’s bodies every day. And if you’re taking more than one medication, supplement, or even herbal tea, you’re already in the mix.
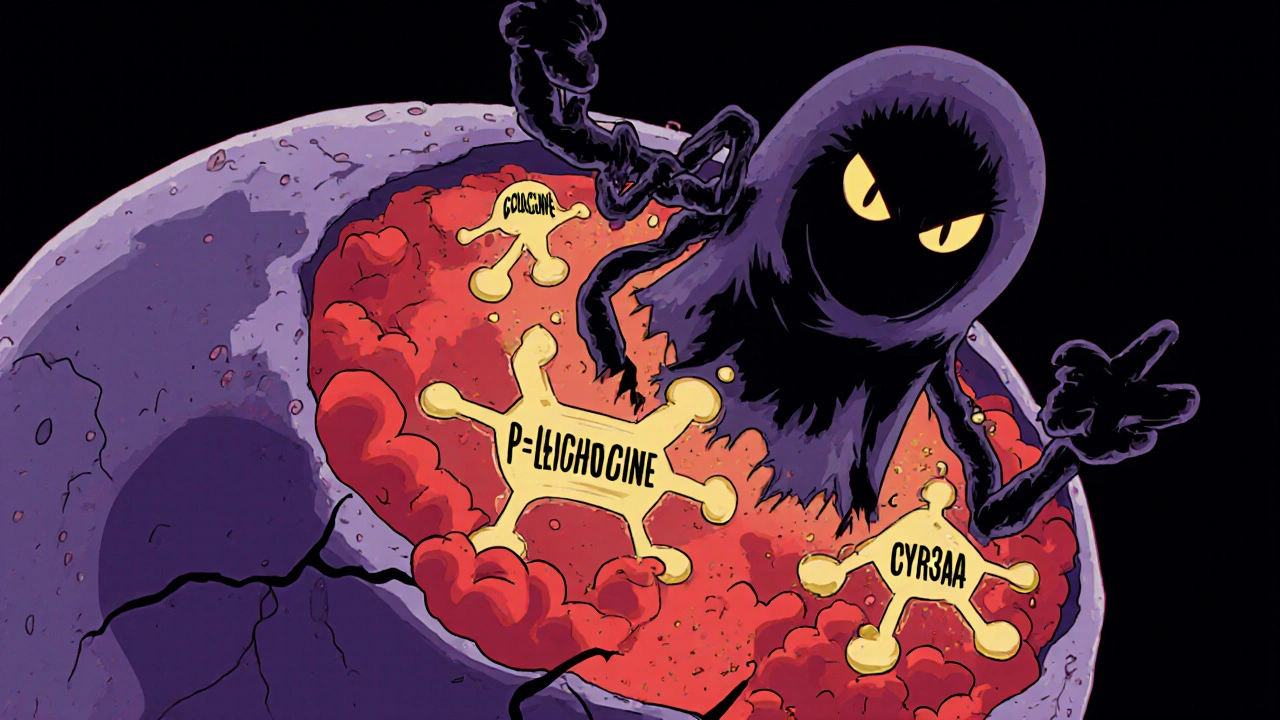
Colchicine and macrolides like clarithromycin can cause deadly toxicity when taken together due to CYP3A4 and P-gp inhibition. Learn which antibiotics are safe, how to avoid life-threatening interactions, and what to do if you've already taken them together.
READ