
Swelling in your hands or feet isn’t always just from standing too long or eating too much salt. If you’ve recently started a new medication, that puffiness could be a direct side effect-and it might be more serious than you think. About 5 to 10% of people on certain drugs experience noticeable swelling in their hands or feet. For some, it’s a mild annoyance. For others, it’s a warning sign that something deeper is going on.
Vasodilator-induced edema is the most common. It happens with drugs like amlodipine (a blood pressure med), nitrates, or gabapentin. This type causes soft, pitting swelling-press your finger on the swollen area and it leaves a dent-that usually starts in the ankles and feet. It gets worse as the day goes on and improves overnight when you’re lying down. Up to 15% of people taking 10mg of amlodipine develop this. If you’re on a higher dose, your risk goes up. At 5mg, it’s closer to 4%.
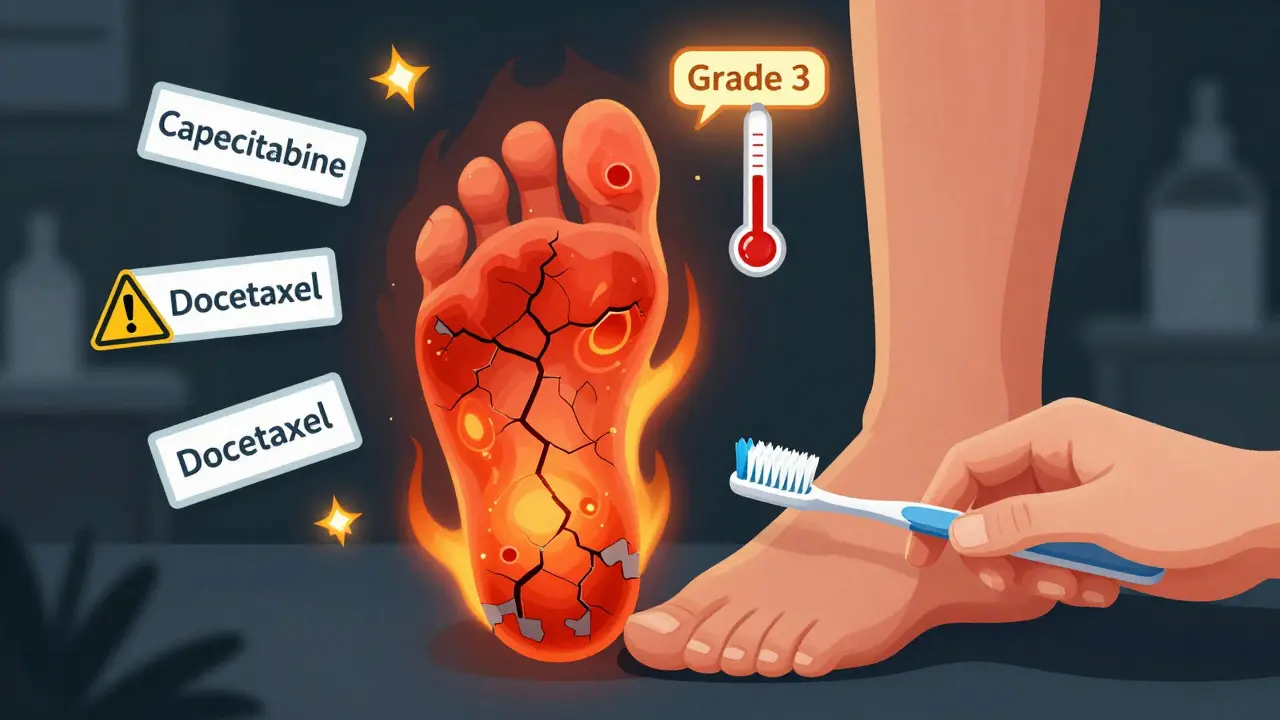
Hand-foot syndrome (also called palmar-plantar erythrodysesthesia) is different. It’s most often caused by chemotherapy drugs like capecitabine. Instead of just puffiness, you’ll notice redness, tingling, numbness, burning, and sometimes blisters or peeling skin on your palms and soles. The American Society of Clinical Oncology grades this from 1 to 4. Grade 1? Mild discomfort. Grade 3? Pain so bad you can’t wash yourself or walk normally. At this stage, it’s not just uncomfortable-it’s dangerous.
If you’re on more than one of these, your risk multiplies. A 2023 review found that patients taking both a calcium channel blocker and an NSAID had nearly double the chance of swelling compared to those on just one.
Call your doctor within 24 hours if you have:
For chemotherapy patients, ASCO guidelines say: if you can’t hold a toothbrush or turn a doorknob because of pain or numbness, contact your oncologist same day. Don’t wait for your next appointment.
And here’s something most people don’t realize: if swelling starts within 72 hours of starting a new medication, there’s a 78% chance it’s caused by that drug. That’s not coincidence. It’s a signal.
Some people try vitamin B6 or arnica gel for hand-foot syndrome. But here’s the truth: a 2022 Cochrane review of eight studies found B6 didn’t help. Arnica gel showed a 28% improvement in one small study, but it’s not widely recommended. Don’t waste time on unproven fixes when proven ones exist.
If it’s a calcium channel blocker causing swelling, they’ll likely:
If it’s hand-foot syndrome from chemo:
But here’s the hard truth: 45% of people still have swelling even after trying all the right steps. Sometimes, the only solution is stopping the drug. That’s not failure. It’s survival.
That delay has consequences. FDA data shows 37% of serious outcomes from drug-related swelling happened because people waited an average of 8.2 days before seeking help. In some cases, untreated swelling led to skin breakdown, infections, or even hospitalization.
On Reddit, someone wrote: “I ignored my swollen feet for two weeks. By the time I went in, I had a blood clot in my leg. Now I’m on blood thinners.” That’s not rare.
On the flip side, people who acted fast often get relief fast. One GoodRx user switched from amlodipine to losartan and had full swelling resolution in five days-without losing blood pressure control.
Swelling from meds isn’t always avoidable-but it’s always treatable. The key is catching it early.
Call your doctor if:
Most cases resolve quickly once the cause is addressed. But waiting too long can turn a simple side effect into a serious health issue. Your swelling isn’t normal. It’s a message. Listen to it.
No. Swelling can also come from heart failure, kidney disease, liver problems, or deep vein thrombosis. But if you started a new medication recently and now have swelling, it’s very likely related-especially if it appeared within 72 hours. Always check with your doctor to rule out other causes.
Yes. NSAIDs like ibuprofen and naproxen can cause fluid retention and swelling in 1-3% of long-term users. Even if you take them only a few times a week for months, your kidneys can start holding onto sodium. If you notice your ankles getting puffy, try switching to acetaminophen and see if it improves.
In most cases, yes. Swelling from calcium channel blockers, NSAIDs, or steroids usually improves within days to weeks after stopping or lowering the dose. For chemotherapy-induced hand-foot syndrome, swelling may take longer to resolve, but it almost always gets better once the drug dose is adjusted. Never stop a medication without talking to your doctor first.
Yes. Graduated compression socks (20-30 mmHg) are one of the most effective non-drug tools. A 2021 trial showed they reduced swelling severity by 40% in patients on blood pressure meds. They work by helping veins push fluid back toward the heart. Wear them during the day, not at night.
No. Hand-foot syndrome isn’t just puffiness-it’s a skin reaction. You’ll see redness, burning, tingling, peeling, and sometimes blisters on your palms and soles. It’s most common with chemo drugs like capecitabine. Regular edema from blood pressure meds is soft, pitting, and doesn’t change skin color or texture. They’re different conditions needing different care.
Not necessarily. Some drugs, like chemotherapy or blood pressure meds, are essential. The goal isn’t to avoid them-it’s to manage the side effect. Your doctor can lower the dose, switch you to another drug, or add treatments like compression or diuretics. Many people continue taking life-saving meds while controlling swelling effectively.
It varies. For calcium channel blocker swelling, most people see improvement in 5-14 days after switching to an ARB or ACE inhibitor. For hand-foot syndrome, it can take 1-3 weeks after dose reduction. In rare cases, swelling lingers for months, especially if skin damage occurred. But 89% of cases fully resolve within four weeks of proper intervention.
14 Responses
This article is basically a glorified drug warning label with footnotes. I’ve been on amlodipine for 5 years and my ankles look like deflated basketballs by 6pm. My doctor said 'it’s normal'-so I just learned to wear loafers. At least now I know I’m not crazy. But seriously, if your doc dismisses this as 'just water weight,' find a new one.
As someone from India where salt is everywhere, this hit home. My uncle took ibuprofen daily for knee pain and his feet swelled so bad he couldn’t wear slippers. Switched to paracetamol and boom-no more puffiness. Simple fix, but nobody tells you this stuff. Thanks for the clarity!
so like... the body is just a glitchy android and meds are the update that bricked it? 🤔
also why is everything a 'clinical trial' or 'cochrane review' like we're in a medical textbook and not reddit?
also also-why does no one ever say 'maybe the drug is just toxic and we're all lab rats'?
STOP. STOP. STOP. I’ve been screaming this for years. People think 'edema' is just 'being chubby' or 'old age.' NO. It’s your kidneys screaming, your heart gasping, your blood vessels drowning. I had Grade 3 hand-foot syndrome from capecitabine-I couldn’t hold my daughter’s hand. And the oncologist said 'take some cream.' That’s not care-that’s negligence. If you’re swollen and your doctor doesn’t adjust your meds, FIRE THEM.
Thanks for this! I’ve been wondering about my swollen toes since starting pregabalin. I thought it was just my shoes. Now I know to track it and talk to my neurologist. Also, compression socks are a game-changer-I got a pair last week and already feel better 😊
Look I get it, but this is just a laundry list of side effects. You’re scaring people into thinking every little puffiness is a death sentence. I’ve had swollen ankles for 3 years, I’m 68, I eat salty food, I sit all day-maybe it’s not the meds? Maybe it’s just gravity and bad lifestyle? Also, why are you promoting diuretics like they’re magic? They dehydrate you and make you dizzy. I’ve seen it. I’ve lived it. This article feels like fearmongering dressed up as science.
Thank you for writing this with such clarity. I’m a nurse and I see so many patients ignore swelling because they're afraid to 'bother' their doctor. This is the kind of info that saves lives. Also-yes to compression socks! I recommend 20-30 mmHg daily. And PLEASE, if you’re on chemo, don’t wait until your skin cracks. Early intervention = less pain. 💙
Pharmacologically, the mechanism is straightforward: vasodilation-induced hydrostatic pressure gradient elevation in the lower extremities due to L-type calcium channel blockade, compounded by sodium retention via RAAS modulation. The clinical significance is often underestimated because of the placebo-driven normalization of symptoms in aging populations. Also, why are we still using 'pitting edema' as a diagnostic term? It’s 2025.
I’m from Nigeria and we don’t have much access to fancy socks or doctors. But I learned from my cousin who took blood pressure pills-he started drinking coconut water and walking every morning. His feet got better. Maybe simple things help too? Not everything needs a trial.
Interesting. But I’m curious-why isn’t there more discussion about the intersection of gender and medication-induced edema? Women are more likely to be prescribed gabapentin, calcium blockers, and corticosteroids. Are we being overmedicated? Or just more visible in reporting? The data doesn’t disaggregate. That’s a gap.
Swelling? Yeah I got it. So what. Drink less water. Move more. Stop being a baby. Your body’s not a damn porcelain doll.
Let’s be real: the pharmaceutical industry doesn’t want you to know that 80% of these side effects are preventable with smarter prescribing. They profit from you suffering, then paying for more drugs to fix the drugs. They don’t care if you can’t walk. They care if you refill. This isn’t medicine-it’s a business model wrapped in a white coat. And we’re all complicit because we trust the system. Wake up.
Oh wow, a whole article about swollen feet. How avant-garde. Next up: 'The Hidden Dangers of Wearing Socks' by the Royal College of Podiatry. Honestly, if you’re getting edema from amlodipine, maybe you shouldn’t have been prescribed it in the first place. Or perhaps your GP just googled 'best BP med' and picked the first one. Either way-this is basic. Why is this trending?
Hey, I’ve been on both amlodipine and gabapentin for years. Swelling started slow. I thought it was just my feet aging. Then I read this and switched to lisinopril. Took 10 days. Swelling gone. No more 'sock marks.' I’m not a doctor, but if you’re reading this and you’re swollen-don’t wait. Talk to your doc. It’s not weak. It’s smart. And hey-if you’ve got compression socks, send me a pic. I need new ones. 😅