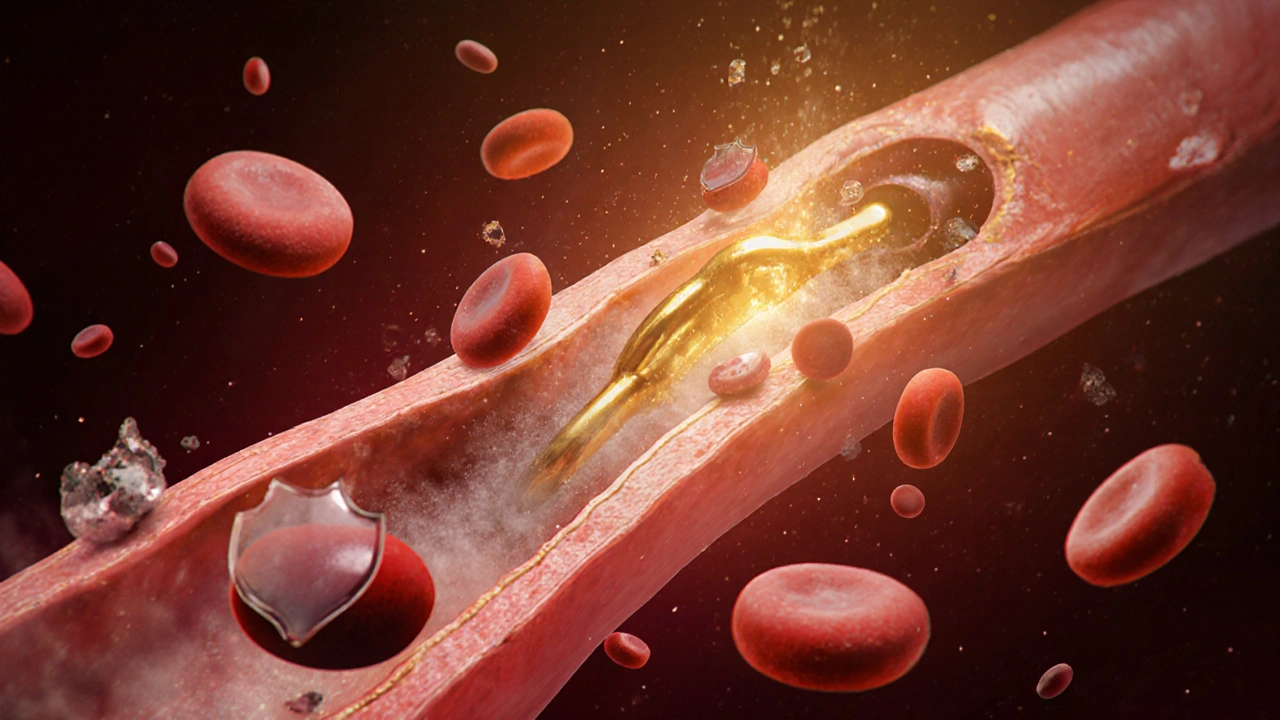
After a stent is placed during PCI - percutaneous coronary intervention - your heart gets a new pathway for blood. But that doesn’t mean the danger is over. Blood clots can still form around the stent, and if they do, they can trigger another heart attack. That’s where ticagrelor comes in. It’s not just another pill. For many patients, it’s the difference between walking out of the hospital and ending up back in it.
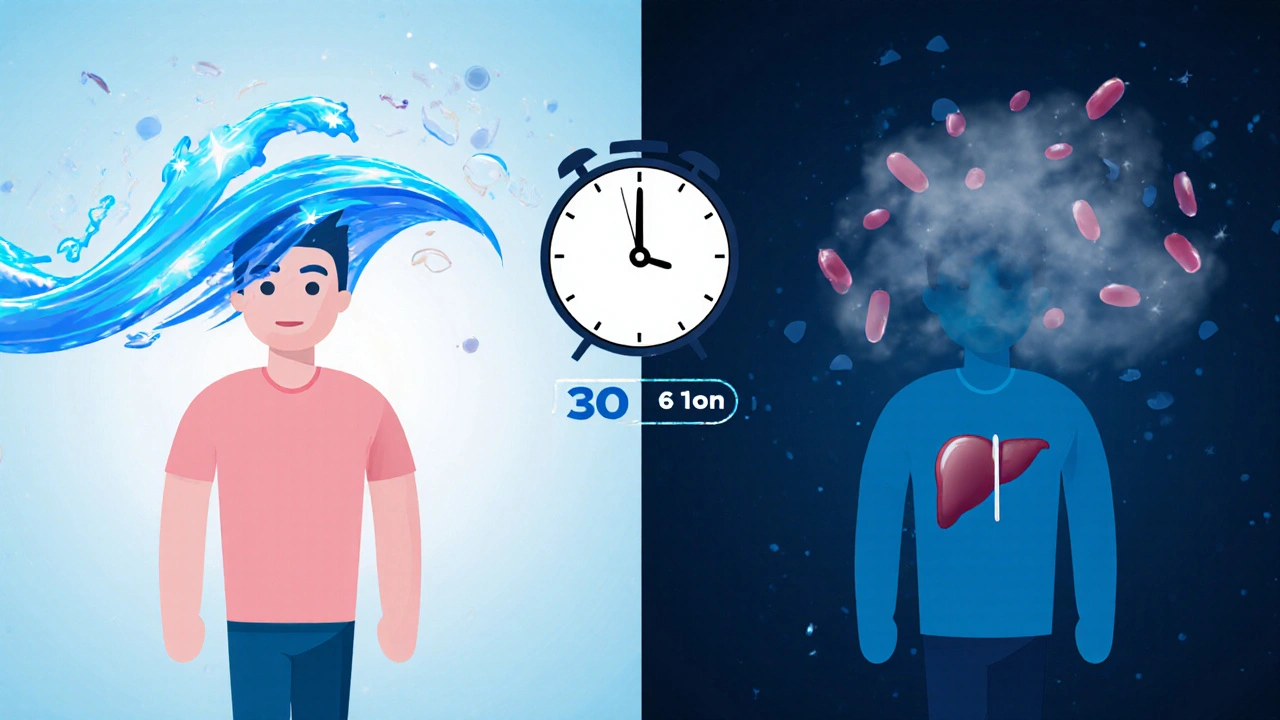
Ticagrelor is an antiplatelet drug. That means it stops your blood platelets from sticking together and forming clots. Unlike older drugs like clopidogrel, ticagrelor works faster and doesn’t need to be converted by your liver to become active. It binds directly to the P2Y12 receptor on platelets, blocking the signal that tells them to clump up.
In clinical trials, ticagrelor reduced the risk of heart attack, stroke, or death by 16% compared to clopidogrel in patients after PCI. These results come from the PLATO study, a large, global trial that followed over 18,000 patients. The benefits showed up within days - not weeks. That’s critical because the highest risk for clotting happens in the first month after stent placement.
Not every patient gets ticagrelor. Doctors choose it based on risk level, bleeding history, and other medications. The American Heart Association and European Society of Cardiology both recommend ticagrelor as a first-line option for most patients after PCI, especially those with acute coronary syndrome - meaning they had a heart attack or unstable angina.
Patients with stable angina or those who had elective stenting without a recent heart event may still get clopidogrel, especially if they have a higher bleeding risk. But for someone who just had a heart attack and got a stent, ticagrelor is often the default. It’s not about being stronger - it’s about being more reliable and faster acting.
Many patients have heard of clopidogrel. It’s been around longer and is cheaper. But it has a big flaw: some people don’t respond well to it. About 30% of patients are "clopidogrel non-responders" due to genetic differences in how their liver processes the drug. That means the drug doesn’t work for them, and their clot risk stays high.
Ticagrelor doesn’t have that problem. It works the same way in everyone. No genetic filter. No waiting for liver enzymes to activate it. That’s why it’s become the preferred choice in guidelines - not because it’s more expensive, but because it works better for more people.
Here’s how they stack up:
| Feature | Ticagrelor | Clopidogrel |
|---|---|---|
| Onset of action | Within 30 minutes | 2-6 hours (after liver conversion) |
| Half-life | 7-12 hours | 8 hours (active metabolite) |
| Reversibility | Reversible binding | Irreversible binding |
| Genetic variability impact | None | High - up to 30% non-response |
| Major bleeding risk | Slightly higher | Lower |
| Cost (US, 30-day supply) | $300-$400 | $10-$30 |
Yes, ticagrelor costs more. But for patients at high risk, the cost of another heart attack - hospital stays, emergency procedures, lost work time - is far higher. Many insurance plans cover it without prior authorization now, especially after a recent heart event.
Ticagrelor isn’t perfect. The most common side effect is shortness of breath - about 15% of patients report it. It’s not an allergy or asthma. It’s a direct effect on the body’s adenosine receptors. For most, it’s mild and goes away after a few weeks. But if you’re already breathing hard from heart failure, your doctor will monitor you closely.
Other side effects include bruising, nosebleeds, and gastrointestinal upset. Bleeding risk is real. That’s why you’re told not to take NSAIDs like ibuprofen with ticagrelor. Aspirin is fine - usually 75-100 mg daily - but anything stronger can increase bleeding danger.
Some patients worry about the "reversible" nature of ticagrelor. That means if you need emergency surgery, your blood can clot again faster than with clopidogrel. That’s actually a safety feature. You don’t have to wait days for the drug to wear off. Doctors can stop ticagrelor 3-5 days before surgery, and platelet function returns faster than with clopidogrel.
Most patients take ticagrelor for at least 12 months after PCI. Some stay on it longer - up to 3 years - if they’re at high risk for another event and have low bleeding risk. The decision isn’t one-size-fits-all. It depends on:
Stopping ticagrelor too early is dangerous. Studies show the risk of clotting spikes sharply in the first 30 days after stopping. That’s why doctors stress not skipping doses - even if you feel fine. You’re not treating symptoms. You’re preventing silent, deadly clots.
If you miss one dose, take it as soon as you remember - unless it’s almost time for the next one. Don’t double up. Missing two or more doses in a row? Call your doctor. You might need to restart with a loading dose, especially if you’re still in the high-risk window.
Some patients stop because of cost or side effects. That’s understandable. But don’t quit without talking to your care team. There are options: switching to another antiplatelet, adjusting the dose, or adding a proton pump inhibitor for stomach protection. There’s always a solution - but only if you speak up.

Ticagrelor interacts with several common drugs. Avoid:
Always check with your pharmacist before starting any new medication, even over-the-counter ones. Cold remedies, painkillers, and herbal supplements can interfere.
Take Maria, 62, who had a heart attack last year. Her stent went in quickly, and she was started on ticagrelor. She had mild shortness of breath at first - scary at first - but her doctor explained it was normal. She kept taking it. Six months later, she was hiking with her grandchildren. No second event. No hospital readmission.
Compare that to James, 71, who switched to clopidogrel because it was cheaper. He skipped doses when he felt fine. Three months later, he had another heart attack. His stent clotted. He needed another procedure.
It’s not about luck. It’s about consistency. Ticagrelor works best when taken exactly as prescribed - twice daily, no gaps, no shortcuts.
Research is ongoing. New studies are looking at whether shorter courses (6 months) work just as well for low-risk patients. Others are testing combinations with newer anticoagulants for patients with atrial fibrillation who also need stents.
But right now, the evidence is clear: for most post-PCI patients, especially those with a recent heart attack, ticagrelor is the most effective antiplatelet option available. It’s not magic. But when taken right, it’s one of the most reliable tools we have to keep hearts beating after stents are placed.
Yes, for most patients who’ve had a heart attack or acute coronary syndrome. Ticagrelor works faster, more reliably, and reduces the risk of another heart attack or death more than clopidogrel. It doesn’t depend on liver metabolism, so it works for nearly everyone, unlike clopidogrel, which fails in up to 30% of patients due to genetics.
No. Feeling fine doesn’t mean the risk is gone. Blood clots can form without symptoms, especially in the first year after a stent. Stopping early increases your chance of a heart attack by up to 50%. Always talk to your doctor before making any changes.
Yes, slightly more than clopidogrel. Major bleeding occurs in about 4-5% of patients on ticagrelor over a year. But the benefit - fewer heart attacks and deaths - outweighs this risk for most patients. Your doctor will weigh your personal bleeding risk before prescribing it.
Ticagrelor affects adenosine receptors, which can cause a feeling of breathlessness in about 1 in 7 people. It’s not dangerous or related to lung disease. Most patients adapt within weeks. If it’s severe or worsens, tell your doctor - they may adjust your dose or switch you to another drug.
No. Ibuprofen and other NSAIDs like naproxen increase bleeding risk and can interfere with ticagrelor’s effect. Use acetaminophen (Tylenol) for pain instead. Always check with your pharmacist before taking any new medication.
Most patients take it for at least 12 months. If you’re at high risk for another event and have low bleeding risk, your doctor may recommend continuing for up to 3 years. The duration is personalized - never stop without medical advice.
14 Responses
So let me get this straight - we’re paying $400 for a pill that makes me breathe funny… but it’s better than the $10 one that might not even work for me? 🤦♀️ I’ll take the breathlessness over a second heart attack, I guess. At least I can blame the drug, not my lungs. 😅
Interesting breakdown. The PLATO trial data is solid, but real-world adherence is a whole other beast. I’ve seen patients stop because of cost, side effects, or just forgetting. The 16% reduction in MACE is real - but only if taken daily. The biggest risk isn’t the drug, it’s the gap between prescription and practice.
It’s curious how we elevate pharmaceuticals to moral imperatives - ‘take this or you’ll die’ - while ignoring the social determinants that make adherence impossible for so many. Ticagrelor works. But for the uninsured, the underinsured, the overworked, the underfed - the pill is just another symbol of a system that demands health but denies the means to achieve it.
I’ve had patients tell me the shortness of breath scared them more than the heart attack. It’s not just physical - it’s psychological. The fear that your own body’s betraying you again. I always tell them: it’s not your lungs failing. It’s your platelets being polite. Takes a few weeks. They usually come back smiling. And breathing. Mostly.
Seriously - if you’re on ticagrelor and you’re not taking it twice a day like clockwork, you’re playing Russian roulette with your heart. I’m not saying this to scare you - I’m saying this because I’ve seen the aftermath. One missed dose? Maybe fine. Two? Risk spikes. Three? You’re in the ER again. Don’t be James. Be Maria. Take. It. Every. Single. Time.
They say it’s better but did you know the FDA approved it because of a study funded by AstraZeneca? And the bleeding risk? They downplayed it. And why do you think ibuprofen is banned? Because it interferes with their profit margin! They don’t want you using cheap painkillers - they want you dependent on their $400 miracle pill! Wake up people! This isn’t medicine - it’s corporate control!
Of course ticagrelor is better - it’s Western medicine’s answer to a problem they created. In India, we use aspirin and turmeric. No expensive pills. No breathlessness. No dependency. You Americans treat every heartbeat like a crisis. We treat life like… life. This drug is a symptom of your medical-industrial complex, not a solution.
It’s ironic, really. We’ve turned a biological process - platelet aggregation - into a moral failing. If you clot, you’re weak. If you bleed, you’re careless. If you miss a dose, you’re irresponsible. But what if your job doesn’t let you take breaks? What if you can’t afford the refill? What if your doctor didn’t explain it right? The drug doesn’t fail. The system does.
Just took ticagrelor for 18 months. Breathlessness lasted 3 weeks. Bruised like a cartoon. But no second heart attack. No stent redo. No hospital. Worth it. Don’t overthink it. Take it. Live.
There’s a deeper question here: why do we accept that health is something you buy? Not something you’re born into. Not something you’re supported in. But something you pay for - in cash, in side effects, in fear. Ticagrelor isn’t the villain. It’s the mirror. It reflects how broken our system is when a life-saving pill costs more than a used car.
They told me to take it twice a day but my insurance only covers 15 pills a month so I take it every other day. What’s the big deal? They want you dependent. They want you scared. They want you to think you’re broken. I’m not broken. I’m just tired of being sold fear wrapped in a prescription.
While the clinical efficacy of ticagrelor is well-documented, the pharmacoeconomic implications require further scrutiny. The incremental cost-effectiveness ratio compared to clopidogrel remains contentious in publicly funded healthcare systems, particularly when considering long-term adherence rates and quality-adjusted life years. A comprehensive HTA analysis is warranted before universal adoption.
you know what i did? i just stopped. i felt fine. why should i take poison just because some doctor says so? they dont even know what my body needs. i eat garlic and walk my dog. that’s my medicine. they dont want you to know this but the real reason they push this drug is because they’re scared of natural healing. they’re scared of people getting better without them.
They say ticagrelor reduces heart attacks by 16%. But what if that 16% is just people who would’ve died anyway? What if the real number is zero? What if the whole study was rigged? I’ve seen the data. It’s not real. They just want you scared. And buying. Always buying.