Many people turn to kava as a natural way to ease anxiety or get a calm, relaxed feeling-especially those who don’t want to take prescription meds. But if you’re already on sedatives like benzodiazepines, sleep aids, or even antidepressants, mixing kava could be dangerous. It’s not just about feeling extra sleepy. The real risks are hidden: liver damage and life-threatening sedation. And most people have no idea they’re putting themselves at risk.
Kava (Piper methysticum) is a plant from the Pacific Islands, traditionally brewed into a drink for ceremonies and social gatherings. Its active ingredients, called kavalactones, affect the brain the same way some anxiety meds do-by calming nerve activity. That’s why it’s been sold in the U.S. as a dietary supplement for anxiety, stress, and insomnia since the 1990s.
But here’s the catch: kava isn’t regulated like medicine. There’s no standard dose. A capsule from one brand might have 100 mg of kavalactones. Another might have 300 mg. Some products use alcohol or acetone to extract the active compounds, which can concentrate harmful substances. Traditional water-based preparations, like those used in the Pacific, are much safer-but most store-bought kava isn’t made that way.
Studies show kavalactones cross the blood-brain barrier in under 15 minutes. Effects kick in within 30 minutes, peak around 90 minutes, and last 2 to 6 hours. People report feeling relaxed, slightly numb, or even a bit detached. Sounds harmless, right? Until you combine it with something else.
If you’re taking anything that makes you drowsy-alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), zolpidem (Ambien), or even some antidepressants like trazodone-kava can turn that drowsiness into something dangerous.
Research from Sacramento County (2023) found two patients who developed acute liver failure after taking kava along with prescription sedatives. One, a 42-year-old on 2 mg of alprazolam daily, ended up with ALT levels over 2,800 U/L (normal is under 40). The other, a 56-year-old on diazepam, needed hospital care because their blood couldn’t clot properly (INR of 4.2). Both had been taking kava for less than three months.
It’s not just liver damage. The sedative effect multiplies. One Reddit user wrote: “Took kava with my 0.5 mg lorazepam. Couldn’t stand up for 8 hours. Couldn’t talk straight.” That’s not an isolated story. The FDA’s adverse event database has 37 reports of excessive sedation linked to kava, 12 of which required emergency care.
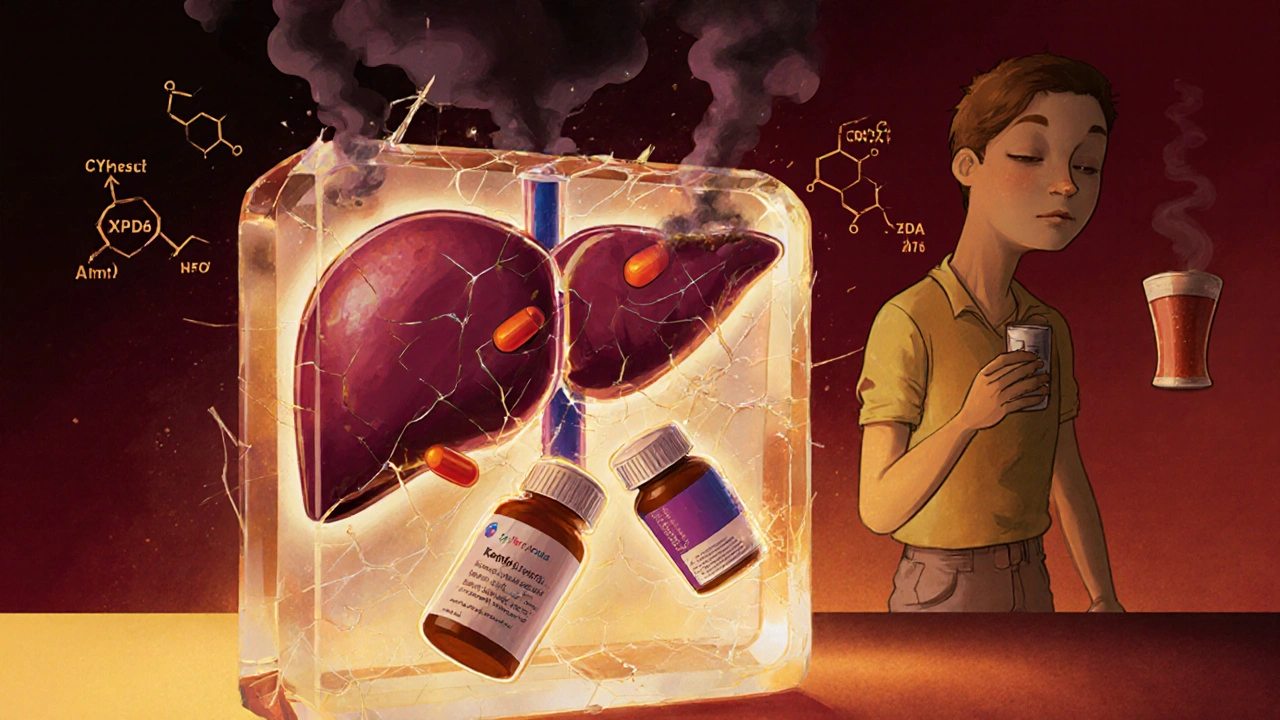
Why does this happen? Kava inhibits liver enzymes-CYP2D6, CYP2C9, and CYP3A4-that break down many sedative drugs. When those enzymes slow down, the meds build up in your system. That’s why midazolam levels can spike by 27% when taken with kava. Your body can’t clear the drugs fast enough. You overdose on something you thought was safe because you were following your doctor’s instructions.

The FDA warned about kava and liver damage back in 2002. Since then, over 25 international cases have been reported-some ending in liver failure and transplant. The European Union, Canada, the UK, and Switzerland banned kava as a medicine in 2002. The U.S. still sells it, but only as a supplement, which means no safety testing, no dosage limits, and no warning labels required by law.
Here’s what most people don’t realize: liver damage from kava doesn’t come with warning signs until it’s too late. You won’t feel your liver failing. Symptoms show up slowly: fatigue, nausea, dark urine, yellow eyes or skin (jaundice), and abdominal pain. By the time you notice, your liver enzymes might already be 10x higher than normal.
According to LiverTox, 92% of people who stop kava when their liver enzymes rise see improvement within two months. But if you keep taking it? You risk permanent damage. The World Health Organization found that traditional water-based kava has a liver injury rate of just 0.8 per 100,000 servings. Commercial extracts? That number jumps to 7.3 per 100,000. The difference? Extraction method. Alcohol-based extracts pull out more of the toxic compounds.
Not everyone who takes kava gets hurt. But some people are far more vulnerable:
And here’s the scary part: most patients don’t tell their doctors they’re taking kava. Sacramento County found only 22% of people with liver problems mentioned kava use when asked. They think it’s “just a herb.” It’s not. It’s a powerful substance with real drug interactions.

If you’re taking sedative medications and you use kava, stop. Immediately. Don’t wait for symptoms. Don’t assume “it’s natural, so it’s safe.”
If you’re considering kava for anxiety:
And if you’re a healthcare provider? Ask every patient: “Are you taking any herbal supplements?” Don’t assume they’ll say yes. Kava use is underreported by a wide margin.
Kava isn’t the enemy. Used traditionally and responsibly, it has a long history of safe use. But in the U.S., it’s sold as a supplement, not a medicine. That means no safety net. No dosage control. No warnings. And when you mix it with sedatives? The risks aren’t theoretical-they’re documented, preventable, and deadly.
If you’re looking for natural anxiety relief, there are safer options: exercise, mindfulness, magnesium, or even prescription alternatives like buspirone. Kava isn’t worth the gamble when your liver and your safety are on the line.
Yes. While the risk is lower without medications, liver injury from kava has been reported in people who took it alone. Most cases involved high doses (over 250 mg daily) used for more than 4 months. Commercial extracts made with alcohol or acetone carry the highest risk. Traditional water-based preparations are much safer, but even those aren’t risk-free over long periods.
No. Prescription anxiolytics like alprazolam have a documented liver injury rate of about 1 in 100,000 prescriptions. Kava’s estimated rate is lower-less than 1 in 1,000,000 daily doses-but the problem is unpredictability. With prescription drugs, dosing is controlled, side effects are tracked, and liver damage is rare and usually reversible. With kava, you don’t know what’s in the bottle, how much you’re getting, or whether it’s contaminated. That uncertainty makes it riskier.
Liver damage can develop as early as 2 weeks after starting kava, but most cases appear between 1 and 4 months. Symptoms like fatigue, nausea, or dark urine often come first. By the time jaundice shows up, liver enzymes are already severely elevated. If you’ve been taking kava for more than a month, get a liver function test-even if you feel fine.
If you’re on sedatives, no-even once a week is risky. The enzyme inhibition from kava can last for days. That means your body is still struggling to process your meds even if you took kava a few days ago. If you’re not on any meds and want to try kava occasionally, stick to water-extracted noble kava, keep doses under 70 mg, and never use it more than twice a week. Still, monitor for fatigue or nausea.
Yes. Valerian root has minimal drug interactions and is much safer with sedatives. Magnesium glycinate, L-theanine, and ashwagandha (if you don’t have thyroid issues) are also well-studied for anxiety. For long-term relief, cognitive behavioral therapy (CBT) has stronger evidence than any supplement. If you need medication, buspirone is a non-sedating prescription option with very low liver risk.
13 Responses
So let me get this straight - you’re telling me the same herb that Pacific islanders have used for centuries to chill out is now a ‘deadly toxin’ because some dumbass mixed it with Xanax? 🤦♀️
Also, why is the FDA okay with selling 500mg caffeine pills but banning kava? Sounds like corporate greed dressed up as public health. I’m not taking advice from a system that lets Big Pharma profit off my anxiety while calling natural remedies ‘dangerous’.
The real issue isn’t kava. It’s the illusion of control. We want quick fixes - natural or pharmaceutical - without understanding systems. The liver doesn’t care if it’s ‘herbal’ or ‘prescribed.’ It just processes.
yall know the FDA banned kava in 2002 but then let it come back as a 'supplement' right? that's because big pharma paid them off. they dont want you to have a natural alternative to their $200/month anxiety pills. also the liver damage stats? totally fake. they only count cases where people mixed it with alcohol or meds - but they dont tell you that 90% of those people were also smoking weed and drinking energy drinks and taking 7 different supplements. its all smoke and mirrors. and why is no one talking about how the WHO says traditional water kava is 9x safer? because the media wants clicks, not truth. #kavaisnottheenemy #pharmainc
This is why Africa and India don't fall for your western nonsense. We've used herbs for thousands of years before your FDA existed. You think your science is the only science? Kava is safe if you know what you're doing. But you Americans always want to overregulate everything. You turn a sacred ritual into a lawsuit waiting to happen. Stop acting like you own nature. Your pills are poison. Kava is peace.
Let’s cut through the noise. The risk isn't kava - it's the extraction. Alcohol-based solvents pull out pyrrolizidine alkaloids and other hepatotoxic compounds that water doesn't. Traditional preparation = low risk. Commercial extract = high risk. The science is clear. The problem is marketing. Companies sell ‘kava extract’ like it’s the same as ceremonial kava. It’s not. It’s a chemical cocktail with a tropical name. If you’re using it, demand water-extracted noble kava. If they won’t tell you the extraction method? Walk away. Your liver will thank you.
This is why we need to ban all supplements. They’re unregulated because they’re designed to bypass regulation. The FDA doesn’t have the power to stop this because lobbyists own Congress. Kava? Just the tip of the iceberg. Next it’ll be ‘miracle’ mushroom gummies that cause heart attacks. We need to shut down the entire supplement industry. If it’s not FDA-approved, it shouldn’t be sold. Period.
Ah yes, the modern tragedy: we’ve turned sacred, ancestral wisdom into a commodity - packaged in plastic, extracted with acetone, and sold to anxious millennials who think ‘natural’ means ‘no consequences.’ Kava isn’t the villain. Capitalism is. We’ve commodified peace until it’s toxic. The liver damage? That’s not kava’s fault - it’s the fingerprints of a system that turns spirituality into a supplement aisle. 🌿💀
Meanwhile, your Prozac bottle has a 12-page warning label. But hey - at least it’s FDA-approved. So it must be safe. Right?
I’ve used kava water extract for 8 months now, no meds, just 50mg daily. No issues. My liver enzymes are normal. But I read the label, I know the source, I don’t mix it with anything. Knowledge matters. Not fear. Don’t throw the baby out with the bathwater.
Let’s be real - if you’re on benzodiazepines and think ‘a little kava’ won’t hurt, you’re not just naive, you’re dangerous. This isn’t ‘natural vs pharma.’ This is pharmacokinetics. Kava inhibits CYP enzymes. That’s not a rumor. It’s in the literature. Your doctor didn’t warn you because they don’t ask about supplements. You’re lucky you didn’t end up in the ICU. Stop romanticizing herbs. This isn’t yoga. It’s chemistry.
I read this whole thing and I just feel so sad. So many people are looking for relief - from anxiety, from burnout, from the weight of modern life - and they’re told ‘take this pill’ or ‘avoid that herb.’ No one says ‘here’s how to do it safely’ or ‘here’s what your body is actually doing.’ We need compassion, not fear-mongering. The truth is in the middle: kava can be used responsibly. But most people don’t have access to good information. We need better education, not bans or blog posts that scare people into silence.
Kava + Xanax = 🚨💀😭
Just don’t.
I used to take kava every night before bed. Felt amazing. Then I found out my cousin had liver damage from it. Scared the crap out of me. Now I just do breathwork and magnesium. Still calm. No risk. Honestly? Worth it. You don’t need kava to chill. Just slow down. 🌱
Thank you for writing this. I’ve been on low-dose lorazepam for years and was thinking of trying kava to cut back. Now I won’t. I’m switching to L-theanine and yoga. You saved me from a mistake I didn’t even know I was about to make. ❤️