
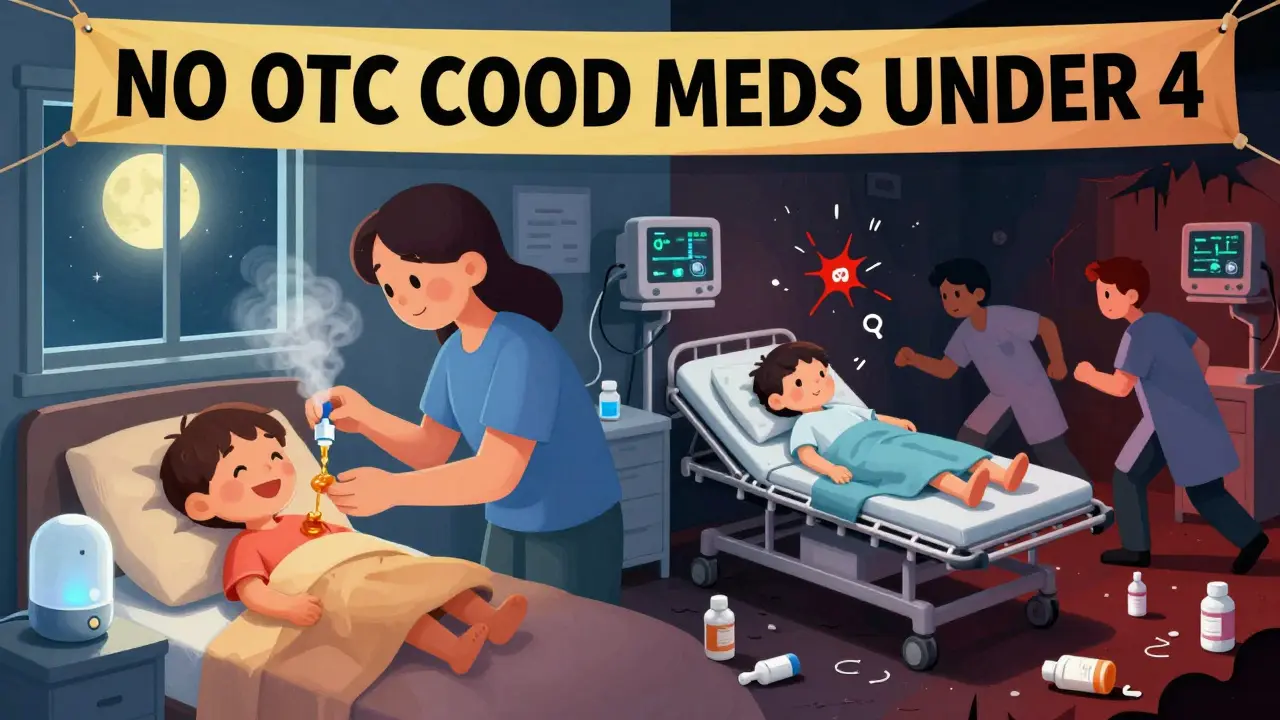
Every winter, parents reach for the medicine cabinet when their child starts coughing or has a stuffy nose. It’s natural to want to help them feel better. But if you’re thinking of giving an over-the-counter (OTC) cough or cold medicine to a child under 4, you’re putting them at risk-without any real benefit.
The U.S. Food and Drug Administration (FDA) and the American Academy of Pediatrics (AAP) have been clear for over 15 years: OTC cold medicines don’t work well in young children, and they can be dangerous. Despite this, many parents still give them. A 2021 survey found that 38% of parents gave these medicines to kids under 4, even though the label says "Do not use." Why? Because they’re desperate. Their child can’t sleep. They’re coughing nonstop. They feel like they have to do something.
Here’s the hard truth: those medicines won’t make the cold go faster. They won’t reduce fever. They won’t stop the cough. And they’ve been linked to seizures, coma, and even death in children under 4.
Most OTC cold products for kids contain a mix of four types of active ingredients:
These ingredients are often combined in one bottle. That’s the biggest problem. Parents don’t realize they’re giving multiple drugs at once. If they’re using a fever reducer like acetaminophen too, they might accidentally overdose. In fact, 68% of dosing errors involve multi-ingredient products, according to a 2020 study in Pediatric Emergency Care.
The rule isn’t arbitrary. It’s based on decades of data.
In 2008, after reviewing hundreds of reports of children getting seriously hurt, the FDA and major manufacturers agreed: don’t use OTC cold medicines in children under 4. That’s not a suggestion. It’s a safety standard. By 2023, every major brand-Children’s Robitussin, Dimetapp, Mucinex-changed their labels to say exactly that.
But why not under 6? Or under 12? Because the data doesn’t support it. A 2012 study in the Journal of the American Medical Association found that 5.2% of all pediatric drug emergencies reported to the National Poison Data System were from cough and cold medicines. Most of those cases were kids under 4 who got into the bottle themselves.
And it’s not just accidental poisonings. Even when parents give the "right" dose, kids react badly. A 2019 study in Pediatrics looked at 1,517 cases of bad reactions between 2004 and 2015. Of those, 65% involved children under 2. More than 70% ended up in the hospital. Common symptoms: fast heartbeat, extreme agitation, trouble breathing.
Age-based dosing is another trap. Kids of the same age can weigh 10 pounds more or less than each other. A 2014 AAP report showed that using age instead of weight leads to dosing errors in 23% to 37% of cases. That’s like giving a full dose to a 20-pound toddler when they only need half.

It doesn’t take much. A teaspoon too much. A second bottle because the first didn’t seem to work. A mix with another medicine.
Overdose symptoms can show up fast:
Poison Control centers in the U.S. received over 12,000 calls between 2019 and 2022 about kids exposed to cold medicines. Over 40% of those were kids aged 1 to 2. Nearly 40% of those cases needed hospital care.
And it’s not just accidental. Some parents give it anyway because they think, "It’s just a little bit." But these medicines affect the central nervous system. A child’s brain and body are still developing. What’s a tiny dose for an adult can be a full dose-or more-for a toddler.
You don’t need medicine to help your child feel better. Here’s what actually works:
These methods are backed by science. They’re safe. And they work.
Confusion. Pressure. Lack of alternatives.
A 2021 AAP survey found that 62% of parents who gave cold medicine to kids under 4 said they did it because they thought a doctor recommended it. But when researchers checked medical records, only 17% had actually talked to a doctor.
Online reviews are mixed. On Drugs.com, parents of kids under 6 gave these medicines an average rating of 1.8 out of 5. Many say, "It didn’t help," or "My child got more agitated." But parents of older kids (7-11) rate them higher-68% say it helped their child sleep. That’s the only real benefit: drowsiness. That’s not healing. That’s sedation.
And the industry knows it. Since 2007, the U.S. market for pediatric cold medicines has dropped from $1.2 billion to $840 million. Manufacturers pulled 37 products off shelves. They’re now focusing on adult formulas and natural alternatives.
The science is clear. The risks are real. But change is slow.
In 2022, the AAP called on the FDA to extend the age restriction to under 6. They also want standardized dosing cups with flow restrictors that limit each dose to 5 mL-something that could cut overdose risk by 82%.
The European Medicines Agency has banned OTC cold medicines for kids under 6 since 2009. Switzerland banned dextromethorphan entirely in 2022.
Research is underway. Nationwide Children’s Hospital is testing lower-dose formulas for kids 2-4 years old. Early results are promising. But until those are approved, the safest rule remains: no OTC cold medicine for children under 4.
Most colds get better on their own in 7-10 days. But watch for these warning signs:
If you’re unsure, call your pediatrician. Don’t guess. Don’t reach for the medicine cabinet. Your child’s safety is worth more than a quick fix.
Leave the cough syrup on the shelf. Your child will thank you when they’re feeling better-without the risk.
12 Responses
I used to give my 3-year-old those little red bottles without thinking. Then one night she went hyper and wouldn’t stop giggling. We ended up at the ER. Never again. 🤦♀️
As a pediatric nurse, I have seen too many children suffer needlessly because of well-intentioned but misguided parental actions. The science is unequivocal: over-the-counter cold medications pose unacceptable risks to children under four. Please, choose safe, evidence-based remedies.
LMAO so now we’re babying toddlers into thinking they need medicine for a sniffle? Next they’ll ban coughing. I gave my kid Robitussin at 2 and he turned into a sleepy angel. The docs are just scared of Big Pharma’s lawsuits. #ParentingWin
I know it’s hard. My daughter had a cough that kept us up for nights. But saline drops and honey? Total game changer. No more panic. No more meds. Just patience and a humidifier. You got this.
I used to think the label was just a suggestion. Then I read the FDA report. Holy crap. I felt so guilty. Now I keep saline and honey in the drawer and everything else locked up. My kid’s still alive. That’s the win.
I’m just saying… if it’s in the medicine cabinet, why NOT use it? I mean, it’s just a little bit. And if it helps them sleep, isn’t that worth it? 😴
The American medical establishment is a corporate puppet. Why do you think they banned these? Because they want you to buy their expensive 'natural' alternatives. Honey? Please. I gave my child syrup since he was 18 months. He’s 12 now. Still breathing.
I’m sorry, but this post is dangerously naive. You’re telling parents to suffer while their children cough? That’s not parenting. That’s neglect dressed up as science. If I want my child to sleep, I’ll give them what works. The FDA doesn’t know my child.
We live in a world where we fear the medicine more than the illness. But what if the real danger isn’t the cough? It’s the fear that makes us reach for chemical solutions instead of presence, warmth, and patience? Maybe the cure isn’t in the bottle-it’s in the hug.
I didn't know about the dosing errors with age vs weight. That's scary. I always used the cup that came with it, but now I'm double checking the mg/kg. Thank you for the info.
Saline drops + humidifier. That’s it.
Oh wow, a whole article about how to not give your kid medicine. Did you get a Pulitzer for this? Next up: 'Why you shouldn't breathe near your baby.'