
Stye is a painful, red lump that appears on the edge of the eyelid, usually caused by a bacterial infection of an eyelash follicle or a gland. It often looks like a tiny pimple and can turn the eye into a raw, watery mess. Chalazion is a firm, painless swelling deep within the eyelid that results from a blocked meibomian (oil) gland. While both cause eye swelling, their origins, symptoms, and treatments differ substantially.
A stye, medically known as hordeolum, can be external (affecting the eyelash follicle) or internal (involving the meibomian gland). The culprit is usually Staphylococcus aureus a common skin bacterium that thrives in warm, moist environments. When the bacteria invade the glandular tissue, the body reacts with inflammation, redness, and a tender bump that may ooze pus.
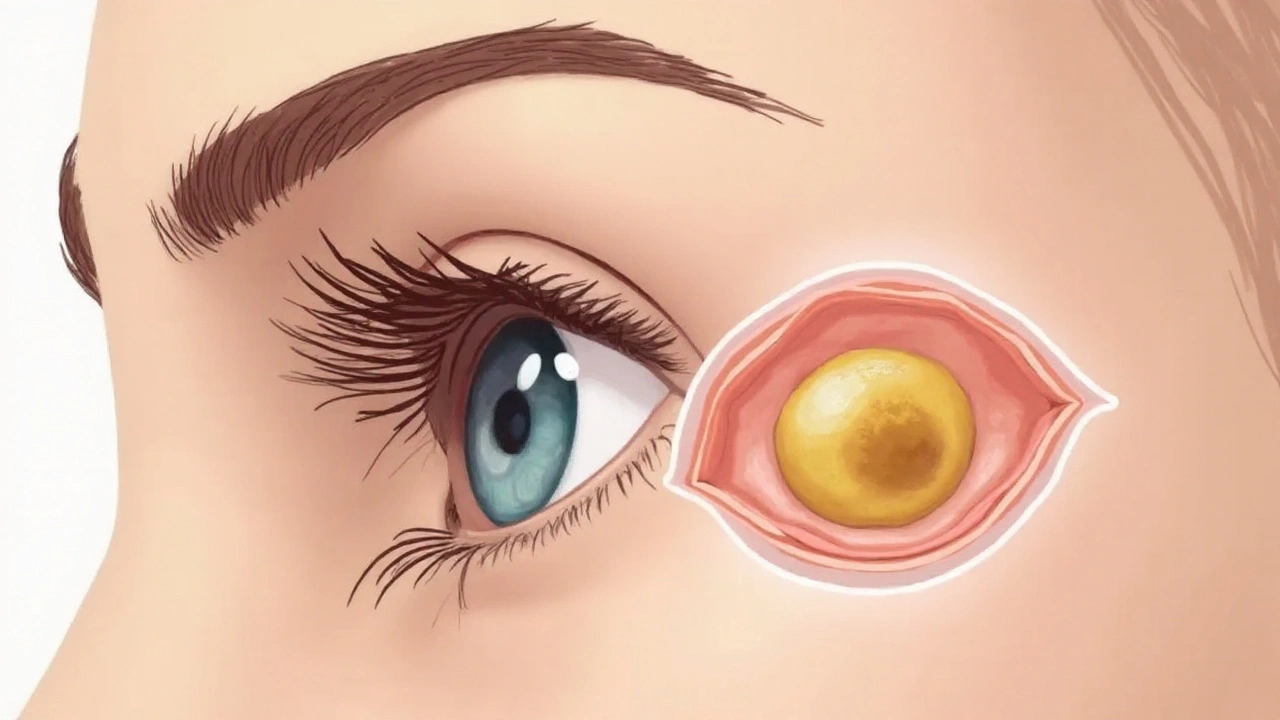
A chalazion, sometimes called a meibomian cyst, forms when the Meibomian gland an oil-producing gland in the eyelid that lubricates the eye surface gets clogged. The blockage causes a buildup of secretions, leading to a solid, often painless nodule. Unlike a stye, infection is rare, and the swelling can persist for weeks or even months if untreated.
| Attribute | Stye (Hordeolum) | Chalazion |
|---|---|---|
| Primary Cause | Bacterial infection of eyelash follicle or gland | Blocked meibomian (oil) gland |
| Typical Location | Edge of eyelid, near lash line | Deeper within eyelid tissue |
| Pain Level | Often painful, throbbing | Usually mild or painless |
| Onset Speed | Rapid, within a day | Gradual, over several days |
| Treatment Approach | Warm compress, hygiene, topical antibiotics if needed | Warm compress, massage, possible surgical drainage |
| Risk of Scarring | Low, if treated early | Higher if chronic |
An Ophthalmologist a medical doctor specializing in eye diseases and surgery uses a slit‑lamp exam to inspect the eyelid at high magnification. They look for signs of pus, erythema, and the exact位置 of the lump. If the lesion is unusually large or non‑responsive, they might order a small biopsy to rule out other eyelid tumors.
In primary care, a simple visual check combined with patient history often suffices. Key questions include:
Most styes and early chalazia respond to conservative measures. The cornerstone is a Warm compress a clean cloth soaked in hot (not scalding) water applied to the eyelid. Heat softens the clogged material and encourages drainage.
For styes, after the compress, gentle massage along the eyelid can help push the pus toward the surface. If there’s obvious crusting, clean the lid with diluted baby shampoo using a cotton swab.
When a stye shows signs of infection (increased redness, spreading warmth, or worsening pain), a Topical antibiotic eye ointment such as erythromycin or bacitracin applied to the lid margin may be prescribed. Over-the-counter options exist, but they’re less potent than prescription formulations.
Chalazia typically don’t need antibiotics. Consistent warm compresses coupled with lid massage often dissolve the blockage over weeks. If the lump persists beyond two weeks, a doctor may perform a minor procedure.
Seek an ophthalmologist if you notice any of the following:
In the clinic, the doctor may perform an Incision and drainage a minor surgical procedure where a tiny cut is made to release pus or clogged oil. The process is quick, often under topical anesthetic, and provides immediate relief for stubborn styes. For chalazia, a single incision and expression, sometimes followed by a brief course of oral steroids, can shrink the nodule dramatically.
Both conditions share risk factors that are easy to manage:
By keeping the eyelid margin clean and the oil flow unobstructed, you reduce the odds of both styes and chalazia forming.
Occasionally, swelling around the eye may stem from other issues:
If symptoms align more with these conditions than a classic stye or chalazion, prompt medical evaluation is essential.
A stye and a chalazion stem from different glands, so one doesn’t directly become the other. However, an untreated internal stye can cause blockage of the meibomian gland, eventually leading to a chalazion‑like cyst.
No. Popping can spread bacteria, worsen inflammation, and increase scarring risk. Warm compresses and gentle massage are the recommended first‑line methods. If it doesn’t drain, let a doctor handle it.
With consistent warm compresses, many chalazia shrink within 2‑3weeks. Persistent lesions may need a minor incision or steroid injection, extending resolution to a few weeks more.
OTC options are limited to warm compress kits and lid scrubs. No creams or ointments directly dissolve the blockage; they only address secondary inflammation. If the chalazion doesn’t improve, a prescription or procedural approach is needed.
A diet low in omega‑3 fatty acids can affect meibomian gland secretions, making chalazia more likely. While diet isn’t a direct cause of styes, overall skin health and immune function-both influenced by nutrition-play a role in susceptibility.
12 Responses
The distinction between a stye and a chalazion is not merely academic; it has direct therapeutic implications. A stye, being an acute bacterial infection, demands prompt antimicrobial measures, whereas a chalazion is a chronic obstructive process that often resolves with persistent heat therapy. Warm compresses should be applied for at least five minutes, three to four times daily; this regimen facilitates liquefaction of the obstructed meibomian secretions. If a lesion persists beyond 48 hours, consider a referral to an ophthalmologist for possible incision and drainage. Proper lid hygiene-using diluted baby shampoo or commercially available lid scrubs-prevents recurrence.
Oh great, another eye bump guide-just what the world needed, right? I mean, who doesn’t love spending all day squinting at a tiny pimple on their lid? Anyway, if yuo’re gonna warm a cloth, don’t burn yourself; we’re not trying to start a new scar‑making hobby. Also, remember that “chalazion” isn’t a fancy French pastry, even though it sounds like one. Stay safe and keep those lids clean-your eyebrows will thank you.
A stye (hordeolum) originates from Staphylococcus aureus infection of an eyelash follicle or gland, leading to rapid onset of pain and erythema. A chalazion, by contrast, is a lipogranulomatous reaction to blockage of a meibomian gland, presenting as a painless nodule that enlarges over weeks. Warm compresses of 40 °C for five to ten minutes, repeated three to four times daily, constitute first‑line therapy for both conditions. Antibiotic ointments are indicated only when purulent discharge is evident. Surgical intervention is reserved for lesions refractory to conservative measures.
What most people don’t realize is that the pharmaceutical industry has a vested interest in keeping minor eye infections alive; think about the endless supply of antibiotic ointments they push. The so‑called “warm compress” recommendation is a low‑cost remedy that keeps you from buying their pricey prescription drops. In reality, many over‑the‑counter products contain hidden steroids that mask symptoms while the underlying blockage worsens. Keep your lids clean, but question every recommendation you see on a corporate‑owned website.
Hey folks! 😊 Thanks for sharing such a detailed guide-I learned a lot about the tiny differences between a stye and a chalazion. 🌟 Remember to replace your mascara every three months; it really helps prevent bacterial buildup. If you’re dealing with a stubborn chalazion, try a warm compress with a fresh, clean cloth every few hours and be patient-most shrink on their own. Stay hydrated and add some omega‑3 rich foods like flaxseeds to your diet; your eyelids will thank you! 🙌
The eye, a window to our soul, often mirrors the chaos we ignore within. A stye is a superficial eruption, a blazing reminder that neglect breeds infection; a chalazion, however, is a deeper stagnation, a silent protest of blocked pathways. Treating these ailments is less about the physical act of compresses and more about confronting our own tendency to let things fester. When the lid finally yields, it’s a small victory over the inertia that pervades our lives. Keep questioning the surface and you’ll uncover the deeper truths hidden behind the swelling.
Most people assume that a chalazion is just a harmless lump, but that’s a naive simplification. In fact, persistent chalazia can indicate systemic lipid disorders or even early signs of ocular melanoma-conditions that the average consumer never considers. The common advice to “just wait a few weeks” is a disservice; early intervention can prevent long‑term complications. Moreover, the emphasis on warm compresses overlooks the potential for bacterial colonization that may necessitate antibiotics. Question the mainstream narrative and seek a thorough work‑up before settling for comfort.
Great summary! For anyone dealing with a stubborn chalazion, I suggest a gentle lid massage after each warm compress-use clean fingertips and move in a circular motion toward the outer edge. Consistency is key; results often appear after the second week of diligent care. Also, incorporate omega‑3 supplements or fish oil capsules to improve the quality of meibomian secretions. If you notice any increase in redness or pain, don’t delay a professional evaluation. Keep up the good work on lid hygiene; it makes a huge difference.
Sure, because everyone has the time for a daily eye‑philosophy session.
Yeah, like I’m sitting there meditating over my eyelid 🙄.
Your observations are appreciated. It is essential to differentiate between infectious and obstructive lid lesions, as the management strategies diverge significantly. Employing warm compresses consistently, adhering to recommended durations, and maintaining meticulous lid hygiene constitute the cornerstone of conservative therapy. Should the lesion persist beyond the expected timeframe, referral to an ophthalmic specialist is advisable. Thank you for contributing to an informed discussion.
The simple advice about warm compresses masks a larger agenda orchestrated by big pharma and ophthalmic device manufacturers. They profit from selling proprietary heat therapy devices that cost far more than a homemade cloth. Meanwhile, the over‑the‑counter antibiotics they push are often laced with undisclosed steroids designed to keep patients dependent. What the mainstream articles omit is the evidence linking chronic chalazia to dietary imbalances promoted by agribusiness. Omega‑3 supplements are sold at premium prices, yet the same benefits can be obtained from ordinary fish. Furthermore, the recommended frequency of three to four compresses per day aligns conveniently with the marketing push for disposable compress kits. The real danger lies in dismissing persistent lesions as merely cosmetic, because many early ocular melanomas masquerade as chalazia. By encouraging self‑treatment, the medical establishment sidesteps early detection, ensuring a steady flow of patients to high‑cost surgical centers. Even the suggested lid hygiene routines often require specialty cleansers that carry hidden fees. Look closely at the language of the article: it subtly directs readers toward branded products without disclosure. The notion that a stye cannot become a chalazion is also contested; some studies indicate a bacterial cascade that leads to gland blockage. This cascade is precisely why antibiotic stewardship programs are underfunded-they prevent the spread of profitable chronic conditions. If you truly want to protect your eyes, you must adopt a holistic approach, incorporating diet, environmental hygiene, and skepticism toward corporate recommendations. Avoid the allure of quick‑fix gadgets and instead rely on tried‑and‑true home remedies, which are rarely mentioned in profit‑driven publications. Remember, every unchecked lid swelling is a potential foothold for larger systemic issues that the establishment prefers to keep hidden. Stay vigilant, question the source of each recommendation, and share this knowledge so others are not blinded by the glossy brochures.