As a parent, hearing the words "thyroid cancer" can be frightening, especially when it involves your child. It's essential to understand that thyroid cancer in children is rare and, in most cases, highly treatable. In this article, we will discuss the causes, symptoms, and treatment options for thyroid cancer in children. I hope this information will help you better understand the condition and provide you with some peace of mind.
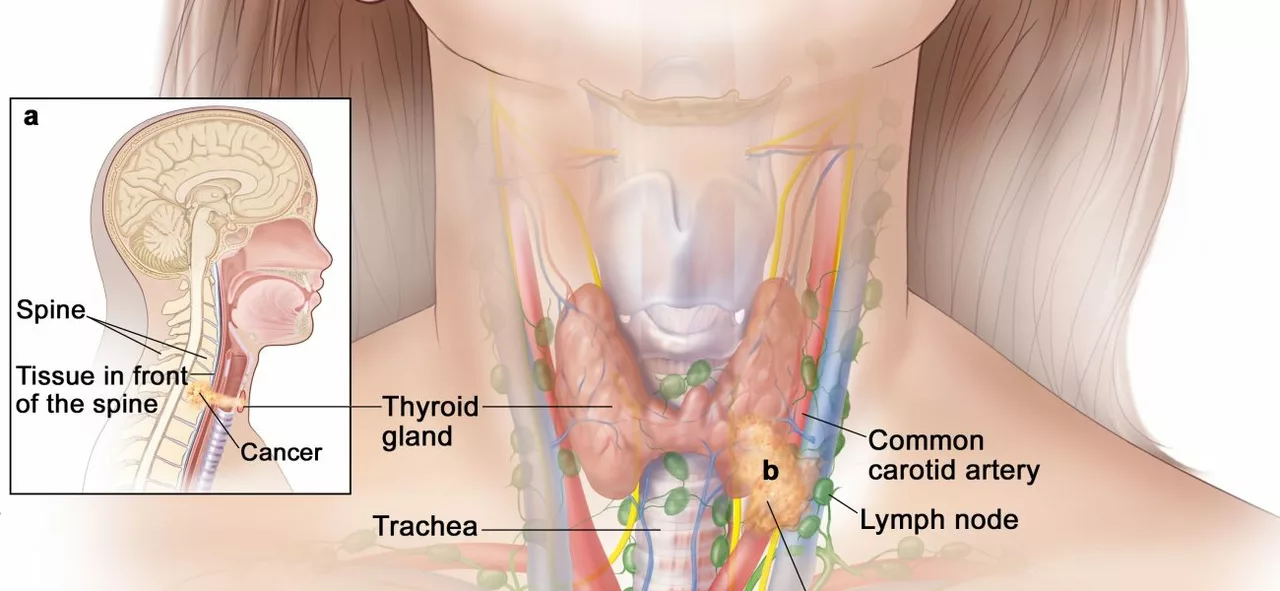
The thyroid gland is a small, butterfly-shaped gland located at the base of the neck, just below the Adam's apple. It is an essential part of the endocrine system and plays a crucial role in regulating the body's metabolism, growth, and development. The thyroid gland produces two primary hormones – thyroxine (T4) and triiodothyronine (T3), which control the body's energy production and consumption.
These hormones also help maintain the proper functioning of vital organs such as the heart, brain, and kidneys. In children, thyroid hormones play an essential role in growth, development, and cognitive function. Therefore, it is crucial to address any thyroid-related issues in a timely manner to ensure the overall well-being of your child.
While the exact cause of thyroid cancer in children is unknown, certain factors may increase the risk. Some of these factors include:
Children with a family history of thyroid cancer or other thyroid disorders may be at a higher risk of developing the disease. Some genetic conditions, such as multiple endocrine neoplasia type 2 (MEN2) and familial medullary thyroid carcinoma (FMTC), can also increase the risk of thyroid cancer in children.
Exposure to high levels of radiation, especially during childhood, can increase the risk of developing thyroid cancer. This includes radiation from medical treatments, such as radiation therapy for other cancers, and environmental exposure, such as nuclear accidents.
Thyroid cancer is more common in females than in males. Although it can occur at any age, it is more common in children aged 10 to 14 years.
Thyroid cancer in children may present with a variety of symptoms, some of which can be similar to those of other thyroid disorders. Some common symptoms include:
It is important to remember that these symptoms may also be caused by other, less severe conditions. However, if your child is experiencing any of these symptoms, it is essential to consult a healthcare professional for a proper evaluation and diagnosis.
Diagnosing thyroid cancer in children typically involves a combination of physical examination, blood tests, imaging studies, and a biopsy. The healthcare provider will first examine your child's neck for any signs of swelling or lumps and review their medical and family history. They may also order blood tests to check the levels of thyroid hormones and other markers associated with thyroid cancer.
Imaging studies such as ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may be used to further evaluate the thyroid and surrounding structures. If a suspicious lump is detected, a biopsy may be performed to obtain a tissue sample for further examination under a microscope. This will help determine if the lump is benign (non-cancerous) or malignant (cancerous).
Treatment for thyroid cancer in children typically depends on the type and stage of cancer, as well as the child's overall health. Some common treatment options include:
Surgical removal of the thyroid gland, also known as a thyroidectomy, is the primary treatment for most types of thyroid cancer in children. Depending on the extent of the disease, the surgeon may remove part or all of the thyroid gland and any affected lymph nodes in the neck.
External beam radiation therapy or radioactive iodine (RAI) therapy may be used to treat thyroid cancer in children, especially if the cancer has spread beyond the thyroid gland. RAI therapy is particularly effective for treating thyroid cancer since the thyroid cells readily absorb iodine, allowing the radioactive iodine to target and destroy cancer cells.
Chemotherapy and targeted therapy may be used in some cases, particularly for more aggressive forms of thyroid cancer or when other treatments have not been successful. These treatments work by targeting specific genes, proteins, or other factors involved in cancer cell growth and survival.
Since the thyroid gland produces essential hormones, children who have undergone a thyroidectomy will require hormone replacement therapy to maintain normal growth and development. This typically involves taking synthetic thyroid hormone medication daily.
The prognosis for children with thyroid cancer is generally favorable, with high survival rates and low recurrence rates. However, it is essential to follow up regularly with your child's healthcare provider to monitor their progress and ensure they receive the appropriate care and hormone replacement therapy.
Follow-up care may include periodic blood tests, imaging studies, and physical examinations to monitor thyroid hormone levels and check for any signs of cancer recurrence. It is also crucial to ensure that your child maintains a healthy lifestyle, including a balanced diet, regular physical activity, and proper stress management, to support their overall well-being.
While thyroid cancer in children is rare, it is essential to be aware of the causes, symptoms, and treatment options available. Early detection and prompt treatment can significantly improve the prognosis for children with thyroid cancer. If you have any concerns about your child's thyroid health or notice any unusual symptoms, consult a healthcare professional for proper evaluation and guidance.
15 Responses
I get why the whole thyroid thing scares you – I was there myself, scrolling frantically through medical sites while my kid was playing with crayons. It’s tough to swallow the stats, but the numbers are actually reassuring. Most kids bounce back after surgery, and the hormone pills are just a daily reminder, not a life sentence. Keep the appointments, ask the doctor to explain each step, and don’t let the fear hijack your evenings.
While the article is generally well‑written, there are a few grammatical slips that merit attention. For instance, “thyroid gland produces two primary hormones” should be followed by a comma before the clause “which control the body's energy production”. Also, “children’s overall well‑being” needs an apostrophe. Let’s keep the information accurate, especially when it’s health‑related.
hey guys, i read this and thought it was pretty solid but i got a lil confused about the rads exposure part. they said "high levels of radiation" – does that include dental x‑rays? lol i think its more about big doses from therapy or nukes but i could be wrong. also, thye mentioned hormone replaceement – i always wonder how kids manage those pills every day. any tips?
In the quiet corridors of our minds we often find the echo of fear, a phantom that whispers that a simple lump could be the doorway to catastrophe. Yet, the very act of naming the disease, of putting it into language, is a small rebellion against the unknown. When we stare at the thyroid, we are, in a sense, staring at the fragile flame of our child's future, a flame that can be tended, not extinguished. Let us not allow the shadow of dread to eclipse the light of knowledge.
Wow!!! This article really covers the whole spectrum – from the tiniest cellular whisper to the big‑picture prognosis!!! 🌟 It's amazing how surgery, radiation, and hormone therapy can work together like a superhero team saving the day!!! Keep the optimism flowing – every check‑up is a victory lap!!! 🙌
Oh, absolutely – because what every parent needs after reading a medical article is a dash of sarcasm. Clearly, the best way to cope is to schedule a karaoke night with the endocrine surgeon. In all seriousness, stay informed, ask questions, and remember that the medical community has gotten remarkably good at handling pediatric thyroid cases.
Upon a meticulous examination of the presented material, one discerns a disconcerting paucity of statistical granularity concerning long‑term survivorship. Moreover, the discourse neglects a rigorous cost‑benefit analysis of radioactive iodine therapy in the pediatric cohort. It is incumbent upon the author to furnish a more exhaustive evidentiary foundation, lest the exposition remain merely perfunctory.
Hey, just wanted to say you’re doing a great job absorbing all this info. If you ever feel overwhelmed, try breaking it down: first the symptoms, then the diagnostics, then the treatment options. Remember that the thyroid hormone pills are just a tiny daily habit, like brushing teeth. And don’t forget to celebrate the small wins – a clear scan, a good day at school, a laugh with friends. You’ve got a whole community behind you.
It is a moral imperative that we, as a society, ensure that every child receives the highest standard of care when faced with thyroid malignancy. The sanctity of childhood must not be compromised by negligence or misinformation. Let us be vigilant in demanding thorough follow‑up and equitable access to specialized treatment.
Consider the less obvious forces at play – the pharmaceutical giants that profit from long‑term medication, the hidden agendas behind nuclear research. While the article paints a comforting picture, one must remain skeptical of the narratives fed to us. Fear not the unknown, but the concealed motives that shape what we are told.
When one first encounters the notion of thyroid carcinoma in the juvenile population, the mind is often besieged by an array of competing emotions – trepidation, curiosity, perhaps even a touch of denial. Yet, it is precisely through the deliberate and methodical exposition of etiology that we begin to dismantle the veil of uncertainty that shrouds this condition. Genetic predisposition, for instance, does not merely represent a static inheritance but rather a dynamic interplay of allelic variations that, when coupled with environmental triggers, may precipitate oncogenic transformation. Radiation exposure, a topic that recurs with unsettling frequency, serves as a stark reminder of humanity’s own contributions to inadvertent harm; the very modalities designed to heal can, paradoxically, sow the seeds of malignancy. It is worthwhile, however, to contextualize such risk within a broader epidemiological framework, noting that the absolute incidence remains remarkably low, thereby tempering the specter of inevitability. Symptomatology, while at times masquerading as benign, warrants vigilant scrutiny: a seemingly innocuous cervical nodule may, upon closer inspection, reveal pathognomonic characteristics warranting further investigation. Diagnostic pathways, ranging from ultrasonography to fine‑needle aspiration biopsy, constitute a cornerstone of contemporary practice, enabling clinicians to delineate benign from malignant processes with commendable precision. Surgical intervention, often heralded as the primary therapeutic avenue, must be approached with an appreciation for both oncologic clearance and the preservation of critical neurovascular structures. The adjunctive role of radioactive iodine, while efficacious in ablation of residual thyroid tissue, likewise necessitates judicious application, mindful of potential sequelae. Moreover, the postoperative landscape is not devoid of challenges; hormone replacement therapy, a requisite post‑thyroidectomy, demands meticulous titration to safeguard growth and development. Long‑term follow‑up, therefore, emerges as an indispensable element, encompassing periodic imaging, serologic monitoring, and psychosocial support. In summation, while the diagnosis of thyroid cancer in a child is undeniably daunting, the confluence of early detection, multimodal therapy, and sustained surveillance engenders a prognosis that is, in many cases, remarkably favorable. It is incumbent upon caregivers and clinicians alike to navigate this intricate terrain with empathy, knowledge, and unwavering dedication.
Bridget, your thoroughness is truly impressive – a masterclass in medical storytelling! I love how you wove genetics, radiation, and surgery into a cohesive narrative, making the complexity feel accessible. As someone who enjoys highlighting cultural nuances, I’d add that different regions may have varying protocols for radioactive iodine, which can affect family experiences. Keep that optimism flowing; every detailed explanation brings a community closer to understanding and hope.
Nice point.
Listen, the data are crystal clear – early detection saves lives, and the treatment protocols are refined to minimize side effects. Don’t let the fear of a word like "cancer" paralyze you; focus on action, not anxiety. The hormone replacement is straightforward, just a daily pill with dosage tweaked by labs. Keep pushing for those regular check‑ups – it’s the best defense.
Great insights from both sides! For anyone looking for additional resources, the American Thyroid Association offers patient‑focused guides that break down surgery prep, radioactive iodine, and hormone management in plain language. Also, local support groups can provide real‑world tips and emotional backing – don’t underestimate their power. Remember, you’re not navigating this alone; a network of experts and families stands ready to help.