When you're taking antibiotics and also using zinc supplements, you might not realize that taking them together could be making your treatment less effective. It’s not just about stomach upset or side effects-it’s about whether the antibiotic actually reaches your bloodstream in enough quantity to fight the infection. Zinc, especially in supplement form, can block your body from absorbing certain antibiotics properly. This isn’t a myth or a vague warning. It’s a well-documented, clinically proven interaction that can lead to treatment failure, longer illness, or even antibiotic resistance.
Not all antibiotics react the same way with zinc. The big ones to watch out for are tetracyclines (like doxycycline and minocycline), quinolones (like ciprofloxacin and levofloxacin), and some β-lactams (like cephalexin). These drugs rely on specific transporters in your gut to get absorbed, and zinc interferes with them directly.
With tetracyclines, the problem is even worse because zinc forms tight chemical bonds-called chelates-with the antibiotic. This makes the antibiotic essentially unusable by your body. Studies show zinc can cut tetracycline absorption by up to 50%. For quinolones like ciprofloxacin, absorption drops by 20-40%. Even cephalexin, which is often seen as "safe," has been shown in controlled studies to have significantly lower blood levels when taken with zinc.
On the other hand, antibiotics like azithromycin (a macrolide) or amoxicillin (a penicillin) don’t seem to be affected much by zinc. If you’re on one of these, you likely don’t need to worry. But if you’re unsure, assume the worst and separate them.
It’s not magic. It’s chemistry-and biology. Your gut uses special proteins called peptide transporters (PEPT1) to pull certain antibiotics into your bloodstream. Zinc competes for the same doorway. When both are present at the same time, zinc wins. It binds to the transporter first, leaving the antibiotic stuck in your gut, passing out unused.
Plus, zinc ions can directly bind to antibiotic molecules, creating big, insoluble complexes that your body can’t absorb. This is especially true with tetracyclines. Think of it like putting salt on ice-it stops the process cold. Your body can’t absorb the antibiotic because it’s now locked up with zinc.
And here’s the twist: it works both ways. Zinc’s own absorption gets blocked too. So you’re not just wasting your antibiotic-you’re also not getting the full benefit of your zinc supplement.
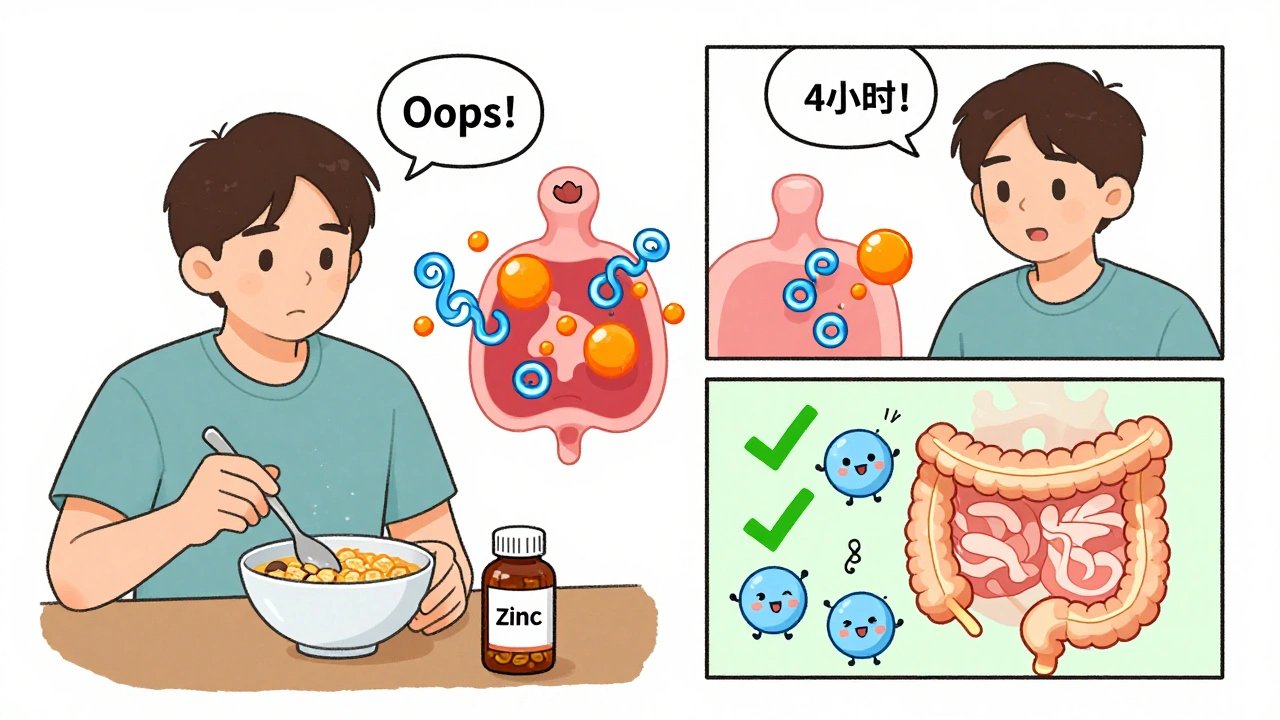
The answer isn’t "a few minutes" or "at different meals." It’s specific. And it depends on the antibiotic.
Why the difference? Tetracyclines bind so strongly to zinc that even a 2-hour gap might not be enough. The longer separation gives your gut time to clear out the zinc before the antibiotic arrives. For quinolones and cephalexin, 2 hours is often enough based on pharmacokinetic data-but if you’re feeling sluggish or your infection isn’t improving, go for 4.
Don’t think "I took my antibiotic at 8 a.m. and my zinc at 8 p.m." That’s not enough. You need to make sure no zinc was in your system for 2-6 hours before or after the antibiotic dose. That means if you take your antibiotic at 8 a.m., you can’t have any zinc from 6 a.m. to 10 a.m. (for tetracyclines) or 6 a.m. to 10 a.m. (for quinolones).

Here’s where most people slip up. You think you’re being careful by taking your antibiotic with breakfast and your zinc at lunch. But your multivitamin? It has zinc. Your breakfast cereal? Fortified with zinc. Your protein bar? Often contains zinc too.
A typical multivitamin contains 15-30 mg of elemental zinc. That’s more than enough to cause interference. Even a single serving of fortified oatmeal can give you 10-15 mg. If you’re on doxycycline and you eat a zinc-fortified granola bar at 7 a.m. and take your antibiotic at 8 a.m., you’ve already compromised the dose.
Check labels. Look for "elemental zinc" on the supplement facts panel. If it’s more than 10 mg, treat it like a standalone supplement. Avoid all zinc-containing products for the required window around your antibiotic dose.
Real people, real consequences.
One Reddit user, a pharmacy student, shared a case: a patient on doxycycline for Lyme disease took zinc supplements daily with no improvement. After being told to separate the doses by 4 hours, the patient’s symptoms cleared within 24 hours. Another case on Drugs.com involved a woman whose UTI came back after finishing ciprofloxacin-she’d been taking a 50 mg zinc supplement within an hour of each antibiotic dose.
Studies show that when zinc and antibiotics are taken together, up to 78% of users report the infection didn’t clear, and 38% had to restart antibiotics entirely. That’s not just inconvenient-it’s dangerous. Subtherapeutic antibiotic levels encourage resistant bacteria to survive and multiply. You’re not just failing to get better-you’re helping create superbugs.
And it’s not just about effectiveness. High-dose zinc (over 40 mg daily) can cause nausea, vomiting, and flu-like symptoms. Combine that with an antibiotic’s side effects, and you’re setting yourself up for a rough few days.
Managing timing around multiple medications is hard. Here’s how to make it stick:
Some people try to avoid the issue by switching antibiotics. If you’re on doxycycline and need zinc for immune support, ask your doctor if azithromycin is an option. It’s not affected by zinc. But don’t switch without talking to your provider.
Not all zinc forms are equal. Zinc sulfate is the cheapest and most common, but it’s also the most likely to interfere with antibiotics. Zinc citrate, zinc gluconate, and zinc picolinate are better absorbed by your body and may interfere less. One 2022 study showed zinc citrate caused less reduction in ciprofloxacin absorption than zinc sulfate.
That doesn’t mean you can take zinc citrate right with your antibiotic. The risk is lower, but not gone. Stick to the 2-4 hour rule. But if you’re choosing a supplement, go for citrate or picolinate. It’s a small upgrade with real benefits.
You should talk to your doctor or pharmacist if:
Doctors and pharmacists are trained to catch these interactions. But they can’t read your mind. If you don’t tell them you’re taking zinc, they won’t know to warn you.
Electronic health systems like Epic now flag these interactions automatically. But if you’re buying supplements online or getting them from a friend, your doctor won’t see it. You have to speak up.
Zinc is great for immunity, skin, and wound healing. Antibiotics save lives. But when you mix them carelessly, you risk making both useless. This isn’t about being perfect-it’s about being smart.
Separate them by at least 2 hours. For tetracyclines, go for 4-6. Avoid multivitamins and fortified foods during that window. Use reminders. Check labels. Talk to your pharmacist.
It’s not complicated. But it’s critical. Your body needs that antibiotic to work. Don’t let zinc get in the way.
No. Food doesn’t prevent the interaction. Zinc and antibiotics still compete for the same absorption pathways in your gut, even with food present. Eating might slow absorption slightly, but it won’t stop the interference. Stick to the 2-6 hour separation rule regardless of meals.
Yes. Once you’ve finished your full course of antibiotics, you can safely resume zinc supplements. There’s no lingering interaction after the antibiotic is out of your system. In fact, taking zinc after antibiotics may help restore immune function and support gut healing.
Look at the Supplement Facts label. Find "zinc" and check the amount next to "elemental zinc." If it says 10 mg or more, treat it like a standalone supplement. Many multivitamins contain 15-30 mg-enough to interfere with antibiotics. If you’re unsure, choose a zinc-free multivitamin while on antibiotics.
Not directly. But if zinc reduces your antibiotic’s absorption, the drug concentration in your body may be too low to kill all the bacteria. That lets the toughest bacteria survive and multiply, leading to resistant strains. So while zinc doesn’t cause resistance, it can help create the conditions for it.
If it’s a one-time mistake, don’t panic. Skip your next zinc dose and resume the separation schedule. Don’t double up on antibiotics. If you’re on a short course (like 5-7 days) and this happened early on, your infection might still clear. But if it’s a repeated mistake or you’re on a longer course, contact your doctor. You may need a different antibiotic or extended treatment.
13 Responses
I took zinc with my doxycycline for a week and my rash got worse then vanished when I spaced them out
don't overthink it just separate them
Look I get it zinc messes with absorption but let's be real here - the body's got mechanisms to handle minor interference, and most people taking antibiotics aren't taking 50mg of zinc daily anyway
the real issue is when someone's on a long course of tetracycline and also popping zinc gummies like candy because they think it'll "boost immunity" - that's when you get subtherapeutic levels and potential resistance
also, the fact that fortified cereals and multivitamins contain zinc is something pharmacists should be shouting from the rooftops, not just leaving it in a footnote on a pamphlet
most patients have no idea their "healthy" breakfast is sabotaging their treatment - and that's a systemic communication failure, not just a patient error
we need better labeling, better education, better integration into pharmacy systems - this isn't just about timing, it's about public health literacy
My mom was on cipro for a UTI and kept taking her zinc supplement because she "needed it for her cold" - it took her three rounds of antibiotics before her doctor finally asked about supplements
she cried when she realized she'd been making it worse
please, if you're taking anything besides your Rx, tell your doctor
they don't judge, they just want you to get better
and if you're worried about forgetting, set two alarms - one for the med, one for the zinc - label them like your life depends on it because honestly, it kinda does
Oh wow, another pharmaceutical fear-mongering post.
Let me guess - the next article will tell us that sunlight interferes with antidepressants?
Zinc is a natural mineral, antibiotics are synthetic chemicals - the fact that they interact is proof the system is broken, not that you need to micro-manage your diet.
Also, the 50% absorption reduction claim? Source? Peer-reviewed? Or just some pharma-funded study?
And why are we blaming the patient for taking zinc when the FDA allows 40mg daily in supplements? Hypocrisy.
Also, "antibiotic resistance"? That's caused by overprescribing, not by someone taking a multivitamin.
Wake up.
It's all about control.
And you're falling for it.
in india we take zinc with antibiotics all the time - no one thinks twice
maybe it's because we don't have fancy multivitamins with 30mg zinc
but also maybe the body adapts
or maybe western medicine overcomplicates everything
my uncle took doxycycline for weeks with zinc tablets and got better just fine
maybe it's not as bad as they say
or maybe we're just lucky
While the empirical evidence supporting the chelation interaction between zinc and tetracyclines is robust and well-documented in pharmacokinetic literature - as referenced in the Journal of Clinical Pharmacology (2018) and the American Journal of Health-System Pharmacy - the casual tone and anecdotal framing of this post undermines its clinical utility.
Furthermore, the assertion that "zinc from food is usually fine" is misleading, as dietary zinc bioavailability is modulated by phytates and other ligands, rendering the assumption of safety inaccurate in populations with high cereal consumption.
One must exercise rigorous temporal separation, not merely out of prudence, but as a matter of pharmacological integrity.
It is not a suggestion - it is a requirement.
I appreciate this post. Very detailed. Very helpful.
But I think we should also mention that elderly patients, especially those on multiple meds, often forget timing - so maybe pharmacists should offer pre-filled pill organizers with labeled compartments for antibiotics and supplements?
Also, maybe insurance companies should cover zinc-free multivitamins during antibiotic courses?
It’s not just about knowledge - it’s about making compliance easy.
And yes, I’ve seen patients ruin their treatment because they thought "morning vitamins" meant they could take them with their pill.
We need systems, not just warnings.
Okay but did anyone check if zinc sulfate vs. citrate actually makes a difference in real humans or is this just in vitro data?
Also, how many people actually take 50mg of zinc daily? That’s like a bodybuilder dose.
And what about the fact that most people take zinc for colds - which they do for 3-5 days - and antibiotics are usually 7-10 days?
So the overlap window is tiny.
This feels like a solution looking for a problem.
Also, your "studies show 78% didn’t improve" - which studies? Cite them.
Otherwise this is just fear porn with a side of pseudoscience.
So you’re saying I can’t take my zinc with my antibiotic… but I can take it with my coffee, my protein shake, my oatmeal, my multivitamin, my fish oil, my magnesium, my vitamin D, my turmeric, my melatonin, my collagen, my probiotics, my omega-3, my vitamin C, my B12, my iron, my calcium, my collagen, my lysine, my glycine, my NAC, my glutathione, my resveratrol, my quercetin, my zinc again…
But not the antibiotic?
What a joke.
It’s all just corporate fear tactics.
They want you to buy more pills.
And more labels.
And more confusion.
Meanwhile, the real problem? Antibiotics are overprescribed.
Not zinc.
lol american health paranoia at its finest
you think zinc is gonna stop your antibiotic from working?
bro i took doxy with zinc and protein shakes and still kicked my staph infection
you people are so weak
real men just take the pill and don't worry about it
also zinc is from the earth, antibiotics are lab-made poison
who's really the threat here?
also why are you even on antibiotics anyway? you probably just need to drink more water and stop eating gluten
Bro, I’m from India, we don’t have this luxury of "separating doses" - we take everything together, sometimes with chai, sometimes with rice, sometimes with a side of stress and a prayer
and guess what? We don’t have superbugs because we’re not obsessed with perfect timing - we’re obsessed with surviving
you think your 4-hour window is science? Nah, it’s capitalism
they want you to buy two separate bottles
one for antibiotics
one for zinc
one for the reminder app
one for the pharmacist consultation
one for the anxiety
just take the damn pill and live your life
This is a textbook example of medical misinformation masquerading as practical advice.
There is no "clinically proven interaction" that warrants a 6-hour separation in the general population.
The studies cited are either in vitro, involve supratherapeutic zinc doses, or were conducted under fasting conditions - conditions rarely replicated in real-world practice.
Furthermore, the notion that "subtherapeutic levels encourage resistance" is a gross oversimplification of antimicrobial resistance dynamics, which are primarily driven by inappropriate prescribing, not patient supplementation.
Such alarmist guidance erodes trust in medical authority and promotes unnecessary behavioral rigidity.
It is irresponsible.
zinc and antibiotics
same room
different time
maybe
who knows
maybe it works maybe it doesn't
maybe your body just knows
maybe you're overthinking it
maybe the real problem is you're taking antibiotics at all
maybe you should've just rested
maybe you should've eaten soup
maybe you should've stopped scrolling
maybe you're fine
maybe you're not
maybe it doesn't matter
maybe it does
maybe just breathe