Antiplatelet Medications: Understanding Bleeding Risks and How to Protect Your Stomach
When you take an antiplatelet medication like aspirin, clopidogrel, or ticagrelor, you're not just preventing a heart attack or stroke-you're also quietly increasing your risk of internal bleeding, especially in your stomach. For millions of people with heart disease, these drugs are life-saving. But for many, the trade-off isn’t clear until they start vomiting blood, passing black stools, or end up in the ER with a dangerous drop in blood pressure. The truth? Antiplatelet medications are one of the most common causes of serious gastrointestinal (GI) bleeding in older adults, and most patients have no idea how to protect themselves.
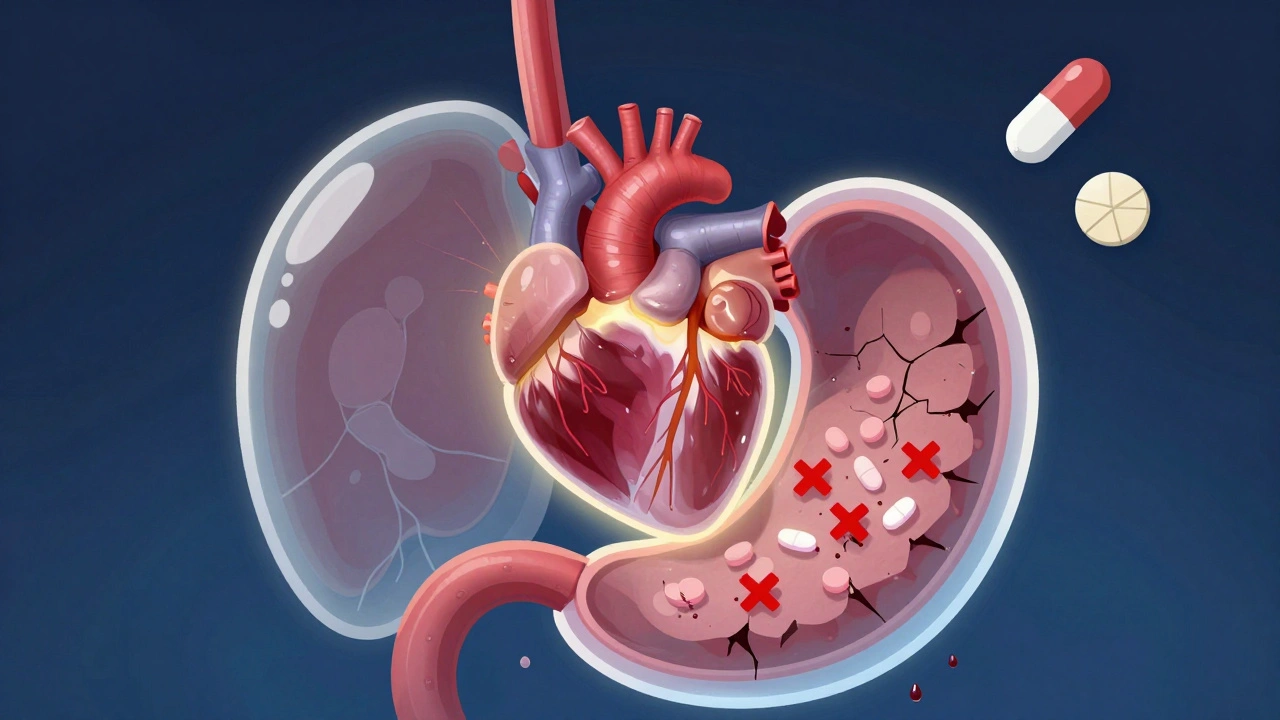
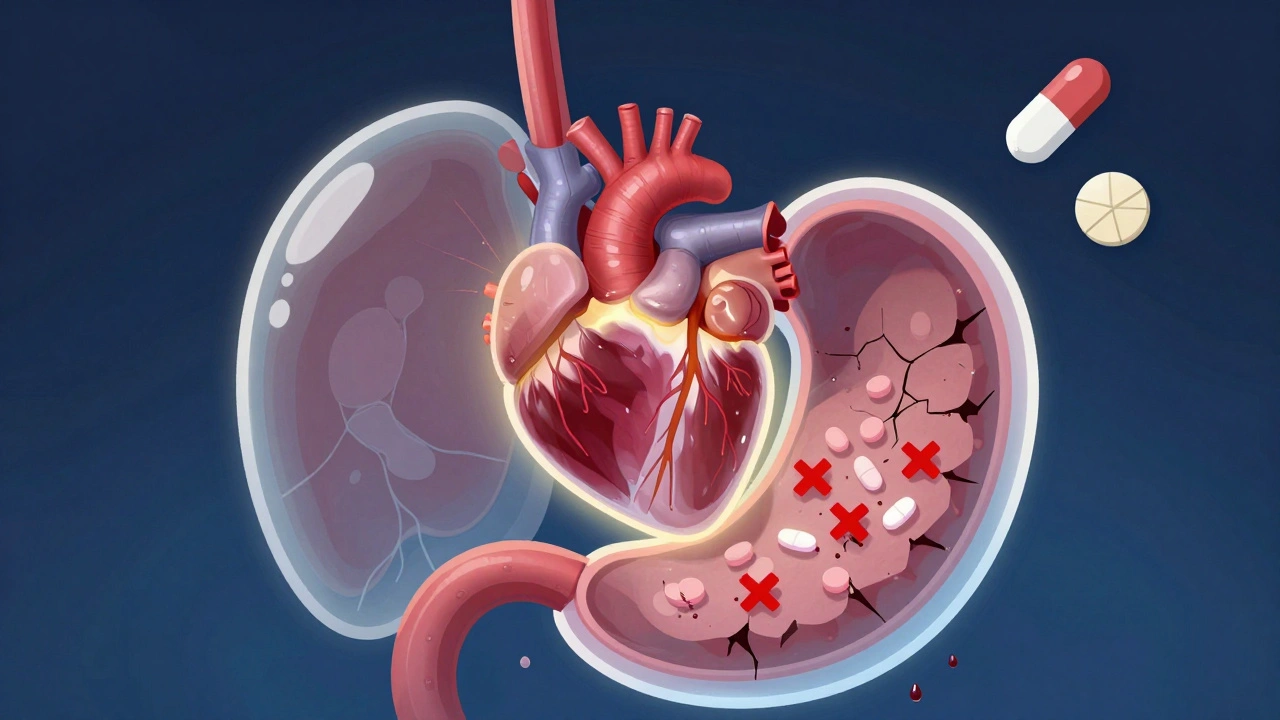
Why Antiplatelet Drugs Put Your Stomach at Risk
These drugs work by stopping your platelets from clumping together. That’s good for your arteries-it stops clots from forming and blocking blood flow. But your stomach lining also needs platelets to repair tiny tears that happen every day from food, acid, and normal digestion. When antiplatelet drugs blunt that repair system, those small injuries turn into ulcers, and ulcers can bleed silently-or catastrophically.
Aspirin is the oldest and most widely used. It’s cheap, effective, and has been around since the 1890s. But even enteric-coated aspirin doesn’t protect your stomach. That coating only delays when the drug dissolves-it doesn’t stop it from affecting platelets throughout your body. A 2023 study found that nearly 40% of people taking aspirin daily developed signs of stomach lining damage within a year, even if they had no symptoms.
Clopidogrel, prasugrel, and ticagrelor are stronger and more targeted. They block a different pathway in platelets, making them more effective at preventing clots after stents or heart attacks. But they’re also harder on the gut. Clopidogrel, for example, doesn’t just inhibit clotting-it also slows the healing of ulcers by reducing growth factors released by platelets. Studies show patients on clopidogrel have nearly twice the risk of developing severe GI injury compared to those on aspirin alone.
And when you combine them-dual antiplatelet therapy (DAPT)-the risk jumps by 30% to 50%. That’s why so many patients on DAPT after a heart stent end up with bleeding complications. The drugs work too well. Your blood doesn’t clot where it shouldn’t… but it also doesn’t clot where it should.
Who’s Most at Risk for GI Bleeding?
Not everyone on these drugs will bleed. But certain factors make it much more likely:
- Age 65 or older
- History of ulcers or GI bleeding
- Taking NSAIDs like ibuprofen or naproxen at the same time
- Having H. pylori infection (a common stomach bacteria that causes ulcers)
- Using steroids or anticoagulants like warfarin or apixaban
- Drinking alcohol regularly
The AIMS65 score is now used by doctors to quickly assess bleeding risk. It looks at five things: low albumin, high INR (a blood clotting test), confusion, low blood pressure, and age over 65. If you score 2 or higher, you’re in the high-risk group. That means you need more than just a warning-you need active protection.
How to Protect Your Stomach Without Losing Heart Protection
The biggest mistake patients make is stopping their antiplatelet drug when they have GI symptoms. That’s dangerous. A 2017 Lancet study showed that stopping aspirin during a GI bleed actually increased the chance of death by 25%. Your heart still needs protection.
The right approach is to keep the antiplatelet drug going-while shielding your stomach. Here’s how:
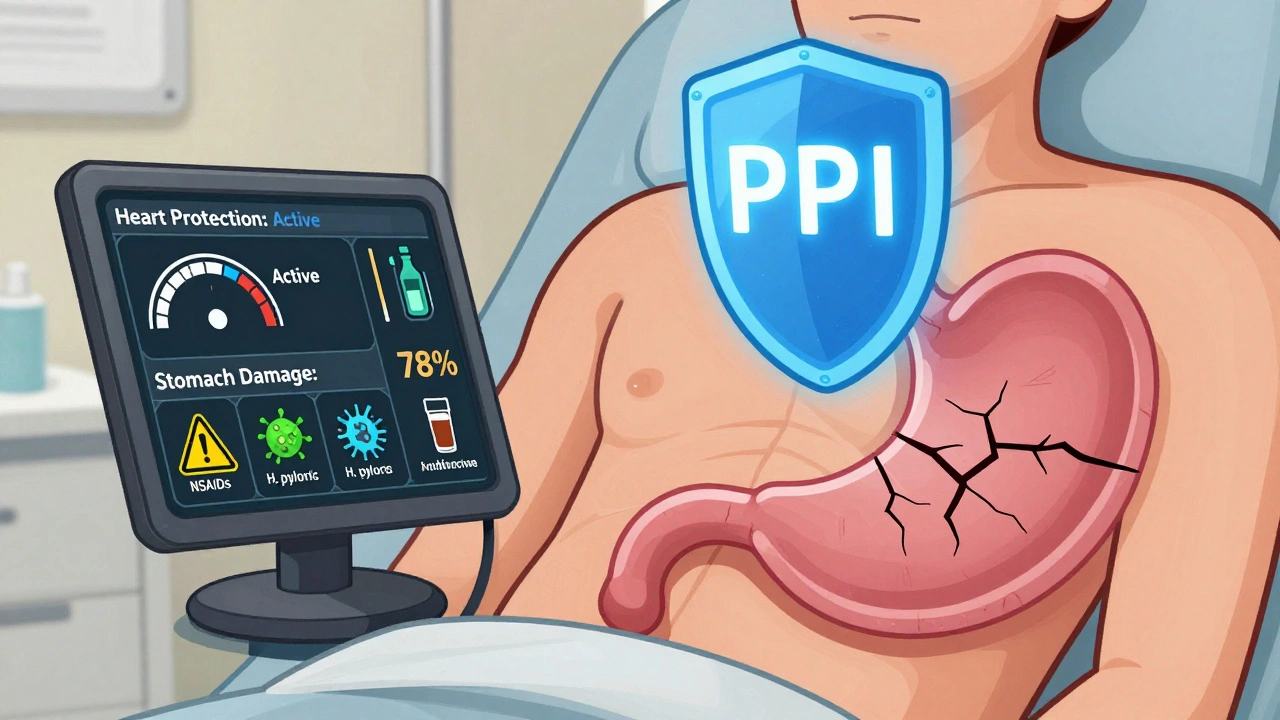
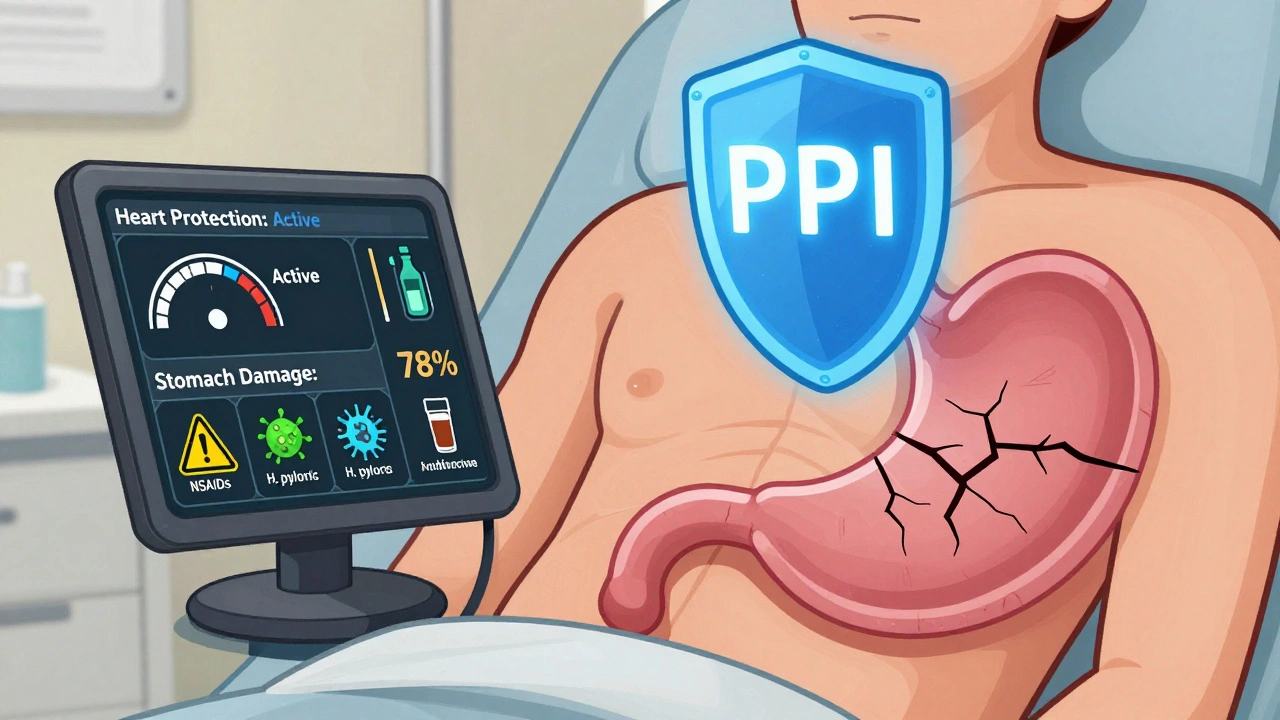
1. Take a Proton Pump Inhibitor (PPI)
PPIs like esomeprazole (Nexium), omeprazole (Prilosec), or pantoprazole (Protonix) are the gold standard. They cut stomach acid by up to 90%, giving your lining time to heal. Studies show that when PPIs are added to antiplatelet therapy, the risk of GI bleeding drops by 50% to 70%.
For high-risk patients, guidelines recommend esomeprazole 40 mg daily. If you’ve had a bleeding ulcer before, you may need to stay on it long-term-even indefinitely.
2. Avoid NSAIDs Like the Plague
Ibuprofen, naproxen, diclofenac-they all damage your stomach lining and make bleeding far more likely. If you need pain relief, use acetaminophen (Tylenol) instead. It doesn’t affect platelets or the stomach lining. And if you’re on a PPI, don’t assume you’re safe with NSAIDs. The combination is still risky.
3. Test for H. pylori
This bacteria is responsible for up to 70% of peptic ulcers. If you’re on antiplatelet therapy and have a history of stomach issues, ask your doctor for a breath test, stool test, or blood test for H. pylori. If it’s positive, a 10- to 14-day course of antibiotics and a PPI can wipe it out-and cut your bleeding risk in half.
4. Don’t Panic About the Clopidogrel-PPI Interaction
You’ve probably heard that PPIs can make clopidogrel less effective. That’s based on a 2009 FDA warning about omeprazole reducing clopidogrel’s ability to block platelets. But here’s the reality: multiple large studies since then have shown no real increase in heart attacks or death when PPIs are used with clopidogrel.
The FDA itself now says the clinical relevance is uncertain. If you’re at high risk for GI bleeding, the benefit of a PPI far outweighs any theoretical risk. If you’re still worried, use pantoprazole or dexlansoprazole-they have the least interaction with clopidogrel.
5. Know When to Call for Help
Watch for these warning signs:
- Black, tarry stools (melena)
- Vomiting blood or material that looks like coffee grounds
- Dizziness, fainting, or rapid heartbeat
- Unexplained fatigue or shortness of breath
These aren’t normal side effects. They’re red flags. Go to the ER. Don’t wait. GI bleeding can kill you in hours if ignored.

What If You’ve Already Had a GI Bleed?
If you’ve bled before, your risk of bleeding again is high-up to 20% in the first year. But you don’t have to stop your heart meds. Here’s what works:
- Continue aspirin. It’s the safest option for long-term use after bleeding.
- Hold clopidogrel, prasugrel, or ticagrelor for 5 to 7 days after the bleed, then restart as soon as your doctor says it’s safe.
- Stay on a PPI for at least 8 weeks after healing, and often longer.
- Never take NSAIDs again.
A 2023 study of 1,200 patients who bled while on antiplatelet drugs found that those who kept aspirin and took a PPI had a 90% lower chance of rebleeding compared to those who stopped all meds.
The Future: Better Drugs, Better Protection
The next generation of antiplatelet drugs is coming. Selatogrel, currently in Phase III trials, shows promise in preclinical studies with 35% less stomach damage than ticagrelor. Researchers are also testing biomarkers-like pepsinogen and gastrin levels in the blood-that could predict who’s most likely to bleed before it happens.
For now, the best strategy is simple: know your risk, protect your stomach, and never stop your heart medication without talking to your doctor.
Frequently Asked Questions
Can I take aspirin if I’ve had a stomach ulcer?
Yes-but only if you’re also taking a proton pump inhibitor (PPI) like esomeprazole. Aspirin is actually the safest antiplatelet drug after a GI bleed. Studies show patients who stay on aspirin with a PPI have far lower rebleeding rates than those who stop it. Never take aspirin alone after an ulcer.
Do I need to stop my antiplatelet drug before a colonoscopy?
Usually not. For most routine colonoscopies without polyp removal, you can keep taking aspirin and even clopidogrel. Stopping increases your risk of heart attack or stent clotting more than the small bleeding risk from the procedure. Only stop if you’re having a major polyp removal or surgery-always check with your cardiologist and gastroenterologist together.
Is it safe to take omeprazole with clopidogrel?
Yes, for most people. Early concerns about omeprazole reducing clopidogrel’s effectiveness have not held up in large clinical trials. If you’re worried, use pantoprazole or dexlansoprazole instead-they have the least interaction. But if you’re at high risk for bleeding, the benefit of a PPI far outweighs any tiny theoretical risk.
Can I use antacids instead of PPIs for protection?
No. Antacids like Tums or Maalox only neutralize acid temporarily. They don’t heal ulcers or prevent bleeding long-term. PPIs reduce acid production for 24 hours and allow the stomach lining to repair itself. Antacids are not a substitute.
Why do I feel bloated or have diarrhea on a PPI?
Long-term PPI use can change your gut bacteria and reduce stomach acid, which helps kill harmful microbes. This can lead to bloating, gas, or diarrhea in 15-20% of users. If symptoms persist, talk to your doctor about switching to a different PPI or lowering the dose. Never stop PPIs suddenly-do it gradually under medical supervision.
What to Do Next
If you’re on an antiplatelet drug:
- Ask your doctor if you’re at high risk for GI bleeding using the AIMS65 score.
- Get tested for H. pylori if you’ve ever had stomach pain or ulcers.
- Confirm you’re on a PPI if you’re on clopidogrel, prasugrel, or ticagrelor-or if you’re over 65 and on aspirin.
- Stop all NSAIDs. Switch to acetaminophen for pain.
- Know the warning signs of bleeding and act fast if they appear.
Your heart needs these drugs. Your stomach needs protection. You don’t have to choose one over the other. With the right plan, you can live longer-and stay out of the hospital.

12 Responses
Stop the PPIs. They cause dementia and bone loss. Your stomach will be fine.
People who take these drugs are just lazy about their diet. Eat clean, stop being a victim. No drug is needed if you're not a junk food zombie.
I had a GI bleed on clopidogrel and was terrified to restart anything. My cardiologist sat with me for 45 minutes and explained the PPI combo. I'm on esomeprazole 40mg daily now and haven't bled again in 3 years. It's not magic, but it's science. Please don't quit your meds because you're scared. Talk to someone who knows the data. You're not alone in this fear.
Let me guess-Big Pharma paid the authors of that 2023 Lancet study. The FDA warning about clopidogrel and PPIs was buried because profits matter more than patient safety. The real cause of GI bleeds? Glyphosate in the food supply. Not aspirin. Not clopidogrel. The system wants you dependent on drugs that mask symptoms while poisoning your gut. Ask yourself: why are PPIs sold as lifelong solutions? Because they're profitable, not because they're curative.
Look, I'm Nigerian and we don't have access to Nexium or Pantoprazole half the time. My uncle took aspirin for 8 years and never had a problem. He drank palm wine, ate spicy food, smoked like a chimney-and still lived to 82. You Westerners over-medicalize everything. If your stomach hurts, stop eating processed crap. Drink ginger tea. Use turmeric. Your body doesn't need a pharmacy to fix what your diet broke.
Also, H. pylori? We test with a spoon and a mirror. If your tongue is white and your breath stinks, you got it. Boil neem leaves. Swish. Done. No lab needed.
And yes, I know this isn't peer-reviewed. But my uncle's still alive. What's your excuse?
This is one of the clearest, most compassionate explanations of antiplatelet risks I’ve ever read. Thank you for writing this. So many patients are left in the dark until it’s too late. The AIMS65 score is underused-doctors should be screening for this like they do for blood pressure. And the point about not stopping aspirin during a bleed? Crucial. I’ve seen too many patients panic and quit their meds, then have a clot weeks later. You’re right: protect the stomach, don’t abandon the heart. This should be a handout in every cardiology clinic.
As a pharmacogenomics specialist, I must emphasize that CYP2C19 polymorphisms modulate clopidogrel activation by up to 70% in East Asian populations, rendering PPI interactions clinically negligible in poor metabolizers. The FDA’s 2009 warning was based on flawed in vitro assays that failed to replicate in vivo pharmacokinetic dynamics. Moreover, the 2023 meta-analysis in JAMA Cardiology demonstrated a hazard ratio of 0.98 (95% CI 0.89–1.07) for MACE in PPI co-administration cohorts. The real threat is therapeutic nihilism fueled by misinformation. PPIs are not a band-aid-they're a mechanistic intervention in the gastric mucosal repair cascade. If you're concerned about microbial dysbiosis, consider a targeted probiotic like Lactobacillus reuteri DSM 17938, which has shown efficacy in reducing PPI-associated bloating without compromising acid suppression.
Why are we trusting American doctors? In India we use Ayurveda. Giloy juice, amla, and licorice root heal ulcers without killing your liver. PPIs are for weak people. Also, why are we taking drugs from Big Pharma? They are controlled by the USA and Israel. Our grandmas didn't need pills. We should go back to nature.
Oh great, another article telling me I need to take more pills. So now I’m on aspirin, clopidogrel, AND a PPI? What’s next? A probiotic? A magnesium supplement? A daily meditation app? I’m not a pharmacy. I’m a human being trying to live. And now I’m supposed to avoid NSAIDs, alcohol, spicy food, and check my stool color every morning? This isn’t medicine. It’s fear marketing dressed up as science. My stomach’s fine. I don’t need a 12-step program to take a pill.
I’m curious-has anyone here discussed the role of gut microbiome diversity in GI bleeding risk? There’s emerging evidence that low microbial richness correlates with impaired mucosal healing, independent of PPI use. If you’re on long-term antiplatelets, maybe a prebiotic fiber regimen (like resistant starch or inulin) could support mucosal repair alongside PPIs? I’m not saying replace the PPI, but could we layer in something that helps the ecosystem? Just wondering if anyone’s tried it.
I’ve been on dual antiplatelet therapy for 5 years after a stent. Started on omeprazole, switched to pantoprazole after reading about the interaction. I also got tested for H. pylori-positive. Treated it with amoxicillin and clarithromycin. No more stomach pain. I still take Tylenol for headaches. I don’t touch ibuprofen. I drink water, not soda. I walk 30 minutes every day. I didn’t need a miracle. I just followed the damn guidelines. This post is basically the checklist I wish my doctor had handed me in 2019. Simple. Clear. Life-saving. Thank you.
Why are we even talking about this? The real problem is that people don't die from bleeding anymore-they get transfusions and endoscopies. This is just another way for hospitals to make money. If you're old enough to need aspirin, you're old enough to die. Stop coddling the elderly. Let nature take its course. And if your stomach bleeds? Maybe you shouldn't have lived this long anyway.