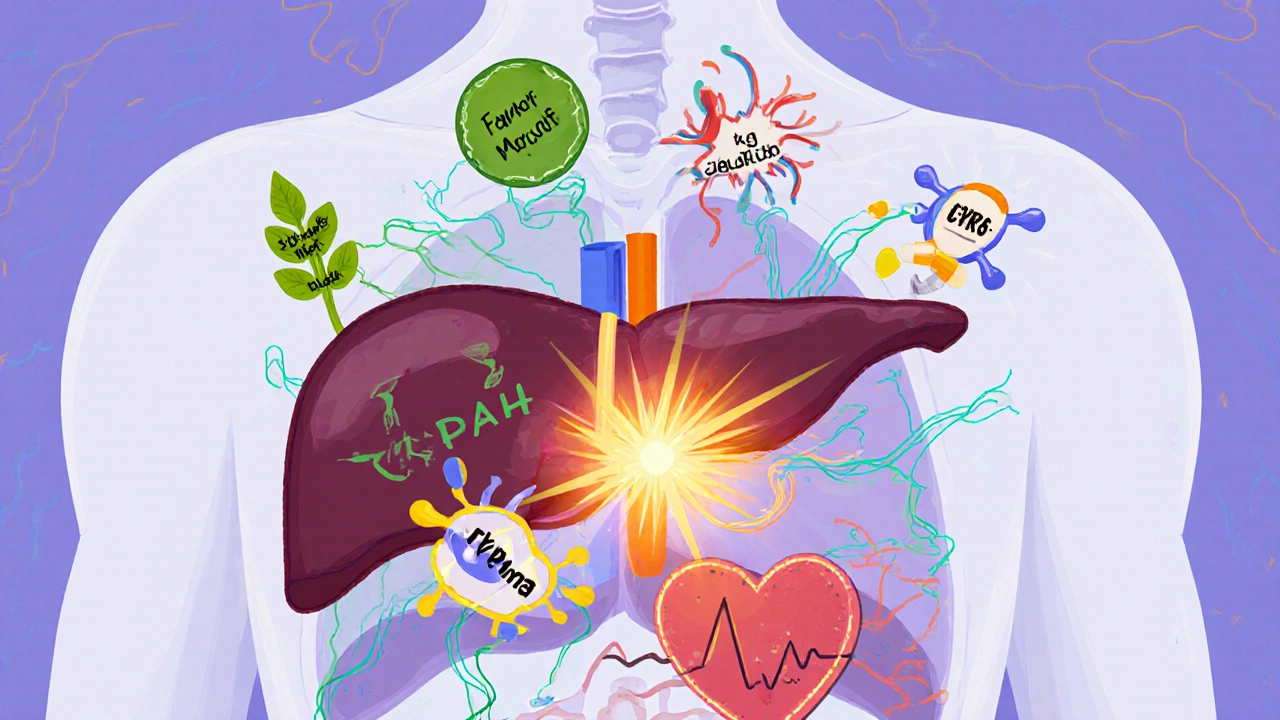
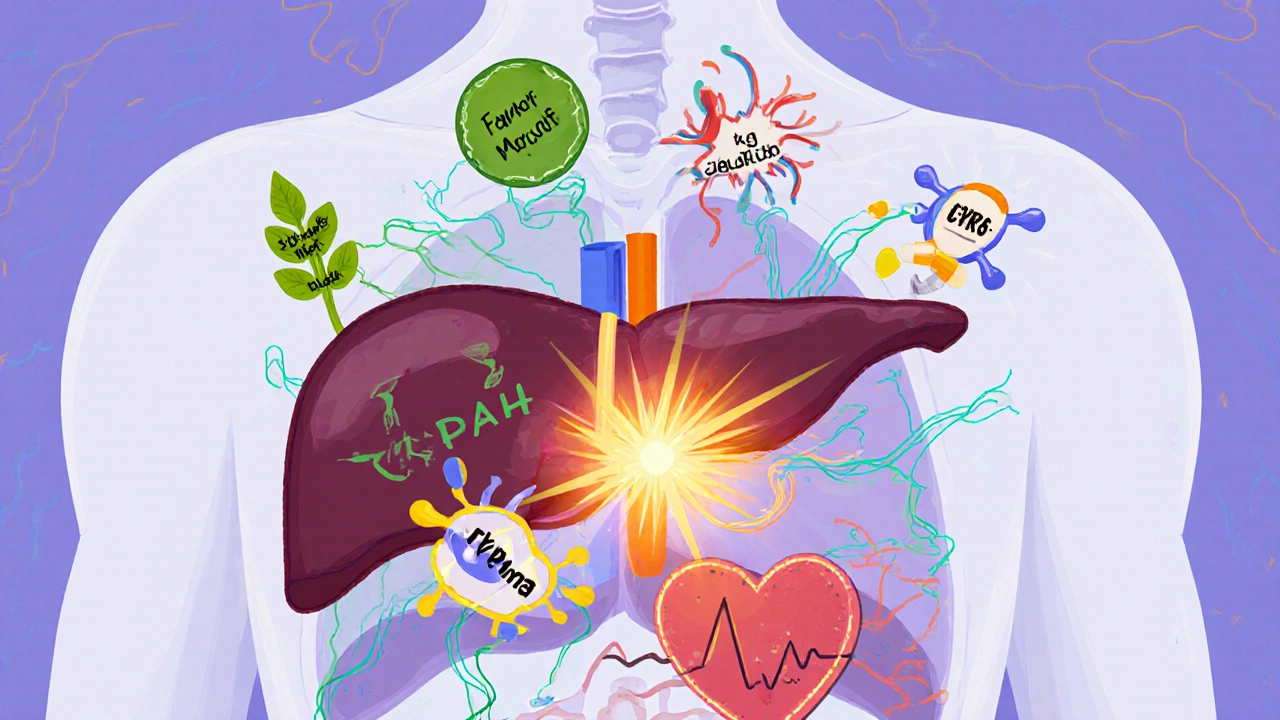
Drug Interactions: How Food, Supplements, and Medications Can Clash

Imagine taking your blood thinner, eating a big salad for lunch, and then popping a garlic supplement-without realizing you’re risking a dangerous bleed. Or popping St. John’s wort for low mood while on your antidepressant, not knowing it could trigger a life-threatening reaction. These aren’t rare accidents. They happen every day, often because people don’t know what’s really going on when food, supplements, and prescription drugs mix.
Why Drug Interactions Are More Common Than You Think
About 40% of American adults take dietary supplements. That’s nearly half the population. And nearly every one of them is on at least one prescription medication. The problem? Most people don’t tell their doctor about the supplements they’re taking. A 2022 study in
JAMA Internal Medicine found that 70% of patients never mention herbal products or vitamins to their providers. That’s a massive blind spot.
The result? Around 3 to 5% of all hospital admissions are linked to preventable drug interactions. That’s tens of thousands of people every year who end up in the ER because something they ate, drank, or took as a pill messed with their medicine. The World Health Organization lists drug interactions as one of the top five medication safety risks globally. This isn’t theoretical. It’s happening right now.
How Interactions Work: Two Main Ways
Drug interactions don’t just happen randomly. They follow two clear biological patterns: pharmacodynamic and pharmacokinetic.
Pharmacodynamic interactions happen when two substances affect the same part of your body-either making each other stronger or canceling each other out. For example, if you take hawthorn (a herbal remedy often used for heart health) along with digoxin (a heart medication), both can boost the heart’s pumping strength. Together, that can push your heart into dangerous overdrive. Or if you take yohimbine (sometimes sold as an energy or libido booster) with a blood pressure pill like guanabenz, they fight each other. One lowers pressure, the other raises it. The outcome? Unstable blood pressure and risk of stroke or heart attack.
Pharmacokinetic interactions are sneakier. They change how your body absorbs, breaks down, or gets rid of a drug. The most common culprit? The liver’s cytochrome P450 enzyme system. It’s responsible for processing about half of all prescription drugs. When something interferes with it, the drug can either build up to toxic levels or get flushed out too fast to work.
Take St. John’s wort. This popular supplement for mild depression is a powerful inducer of CYP3A4, one of the main liver enzymes. When you take it, your body starts breaking down other drugs faster. Studies show it can slash blood levels of cyclosporine (a transplant drug) by 50-70% in just two weeks. That means your body might reject the new organ. It can also make birth control pills useless-raising the risk of unintended pregnancy by up to 70%. And if you’re on an SSRI antidepressant? You could trigger serotonin syndrome: a dangerous spike in brain serotonin that causes fever, muscle spasms, confusion, and even death if not treated immediately.
The Grapefruit Effect: A Food That Can Kill
Grapefruit isn’t just a healthy breakfast choice-it’s a silent drug amplifier. It contains chemicals called furanocoumarins that permanently disable a key enzyme in your gut called CYP3A4. That enzyme normally breaks down certain drugs before they enter your bloodstream. When it’s shut down, the drug floods in.
One of the most dangerous examples is simvastatin, a cholesterol-lowering statin. Eating just one grapefruit can increase simvastatin levels in your blood by up to 15 times. That’s not a little extra-it’s a massive overdose. The result? Rhabdomyolysis: the rapid breakdown of muscle tissue. This releases toxins into your blood that can shut down your kidneys. The risk jumps from 0.15 cases per 100,000 people per year to 1.57 when grapefruit is involved.
And it’s not just grapefruit. Pomelos, Seville oranges, and even some grapefruit juices have the same effect. If your pill bottle says “avoid grapefruit,” don’t assume it’s just a suggestion. It’s a warning.
Leafy Greens and Blood Thinners: The Vitamin K Trap
If you’re on warfarin (Coumadin), your doctor probably told you to watch your vitamin K intake. But most people don’t realize how easy it is to mess this up.
Vitamin K helps your blood clot. Warfarin blocks it. So if you eat a lot of vitamin K one day and almost none the next, your INR (a measure of how long your blood takes to clot) swings wildly. A 2018 study found that eating just 150 grams of cooked spinach-about a cup and a half-can drop warfarin’s effectiveness by 30-40% within 24 hours. That’s enough to raise your risk of stroke or blood clots.
The solution? Don’t avoid spinach. Just keep it consistent. If you eat spinach every day, your body adjusts. If you eat it once a week, your INR will jump and drop unpredictably. The National Academy of Medicine recommends 90 mcg of vitamin K daily for women and 120 mcg for men. That’s about one serving of kale, broccoli, or spinach. Stick to that amount. Don’t go wild. Don’t go cold turkey.
And don’t forget cranberry juice. Despite being “healthy,” it’s been linked to over 28 documented cases of dangerous bleeding in people on warfarin. INR levels spiked above 8.0-way beyond the safe range of 2.0 to 3.0. Green tea? Also high in vitamin K. Same risk.
Supplements That Are More Dangerous Than You Think
Not all supplements are harmless. Some are basically unregulated drugs.
Ginkgo biloba is sold for memory and circulation. But it also thins the blood by blocking platelet-activating factor. When combined with warfarin, aspirin, or even NSAIDs like ibuprofen, it can double your bleeding risk. Studies show it can extend bleeding time by 30-50%. One case report described a man who developed a brain bleed after taking ginkgo with aspirin.
Garlic supplements work the same way. A 2001 study found 32 cases of abnormal bleeding in people taking garlic with blood thinners. Some needed emergency transfusions.
Red yeast rice sounds natural-because it is. But it contains monacolin K, which is chemically identical to lovastatin, a prescription statin. Taking it with a prescription statin? You’re doubling your dose. That raises your risk of muscle damage (myopathy) by 2.3 times, according to a 2017 study in the
Journal of the American College of Cardiology.
Coenzyme Q10 is often taken for heart health or to reduce statin side effects. But research suggests it might actually reduce statin effectiveness. If you’re taking both, your cholesterol might not be under control-and you won’t even know.

What You Can Do Right Now
You don’t need to be a pharmacist to protect yourself. Here’s what works:
- Make a complete list of everything you take: prescription drugs, over-the-counter meds, vitamins, herbs, and even occasional supplements like melatonin or fish oil. Update it every time you see a doctor or pharmacist.
- Ask your pharmacist every time you pick up a new prescription: “Could this interact with anything I’m already taking?” Pharmacists are trained to catch these things. A 2022 study showed pharmacist-led reviews reduce adverse events by 22%.
- Use free tools. The FDA’s MedlinePlus Drug Interaction Checker lets you enter up to 10 medications and supplements at once. It’s free, reliable, and updated regularly.
- Don’t assume “natural” means safe. Just because something comes from a plant doesn’t mean it won’t hurt you. St. John’s wort, ginkgo, and garlic are all natural-and all carry serious risks.
- Report bad reactions. If you think a supplement caused a problem, report it to the FDA’s MedWatch program. Every report helps build better safety data.
What Doctors and Pharmacies Are Doing About It
Health systems are waking up. Hospitals using electronic health records like Epic now have built-in interaction alerts. One study found these alerts cut dangerous prescribing by 37%. Pharmacists are now trained to ask about supplements during every medication review. The American Pharmacists Association says this reduces costs by over $1,100 per patient per year.
The FDA is pushing for better labeling on supplements. Right now, only 29% of supplement bottles include any interaction warning. Compare that to prescription drugs, where warnings are mandatory. A 2023 draft FDA guidance now requires new drugs to be tested for interactions with common supplements like St. John’s wort and garlic.
And researchers are using AI. IBM Watson Health’s pilot program analyzed 10 million clinical notes and predicted new drug-supplement interactions with 87% accuracy. That’s not science fiction-it’s happening now.
Final Thought: Your Safety Is Your Responsibility
Medications save lives. But they can also harm you if you don’t understand how they behave in your body. Food and supplements aren’t bystanders-they’re active players. A salad, a capsule, a glass of juice-they can all change how your medicine works.
The best defense? Talk. Write it down. Ask. Don’t assume your doctor knows what you’re taking. Don’t assume your supplement is harmless. And don’t wait until something goes wrong to find out.
Your health isn’t just about what you take-it’s about how everything you take works together.
Can I still eat grapefruit if I’m on a statin?
No, if you’re taking simvastatin, atorvastatin, or lovastatin, avoid grapefruit entirely. Even small amounts can cause dangerous spikes in drug levels. If you’re on rosuvastatin or pravastatin, grapefruit is generally safe. Always check with your pharmacist or doctor-don’t guess.
Is it safe to take St. John’s wort with antidepressants?
No. St. John’s wort can cause serotonin syndrome when taken with SSRIs, SNRIs, or other antidepressants. Symptoms include high fever, rapid heart rate, muscle stiffness, confusion, and seizures. This is a medical emergency. Never combine them without explicit approval from your doctor.
Do I need to stop all supplements if I’m on blood thinners?
Not all, but many. Avoid ginkgo, garlic, ginger, high-dose vitamin E, and fish oil unless approved by your doctor. You can still eat leafy greens-but keep your intake consistent. Sudden changes in vitamin K can cause your INR to swing dangerously.
Can I use herbal supplements if I have a chronic condition?
It’s risky. People with heart disease, diabetes, liver disease, or autoimmune conditions are especially vulnerable to interactions. Herbs like echinacea, black cohosh, and saw palmetto can interfere with immune drugs, blood sugar meds, and hormone therapies. Always consult your doctor before starting any new supplement.
How do I know if a supplement is interacting with my medication?
Watch for sudden changes: unusual bruising or bleeding, muscle pain or weakness, dizziness, confusion, irregular heartbeat, or worsening symptoms. If you start a new supplement and feel worse, stop it and call your doctor. Don’t wait. Many interactions develop within days.
Are there apps or tools to check for interactions?
Yes. Use MedlinePlus Drug Interaction Checker (free, from the U.S. National Library of Medicine). Also try the FDA’s Drug Interaction Checker or Epocrates (for healthcare professionals). Always cross-check with your pharmacist-even the best apps can miss rare interactions.
Why don’t supplement labels warn about interactions?
Because under U.S. law, supplements aren’t required to prove safety or efficacy before selling. Unlike prescription drugs, they don’t need FDA approval. Only 29% of supplement labels include interaction warnings. The FDA is pushing for change, but progress is slow. Until then, assume every supplement has risks.

15 Responses
bro i just took garlic pills with my blood thinner and now i'm scared to poop lmao 😅
this is why you talk to your pharmacist. they don't get paid enough to care but they know way more than your doctor about what's in your cabinet. i used to take red yeast rice with my statin until my pharmacist called me out. now i just eat oats. simple.
The sheer negligence exhibited by the lay public in self-administering phytochemical compounds without regard for pharmacokinetic modulation is not merely alarming-it is an indictment of modern medical illiteracy. One cannot, with any semblance of intellectual integrity, presume that botanical extracts are benign merely because they are derived from flora. The CYP450 system does not discriminate between pharmaceuticals and herbalism; it metabolizes indiscriminately, and the consequences are neither theoretical nor anecdotal-they are statistically catastrophic.
I’ve been on warfarin for eight years, and I eat spinach every single day. Same amount. Same time. My INR is stable. The key isn’t avoidance-it’s consistency. People panic over change. Your body doesn’t. It just wants routine.
This article is basically just fearmongering dressed up as education. Most people don’t even know what CYP3A4 is. You’re scaring folks into thinking their chamomile tea is going to kill them. The real danger is overmedication-not supplements.
I think it's irresponsible to suggest that people should just 'ask their pharmacist' without acknowledging that many pharmacies are understaffed, overworked, and underpaid. The burden of safety is being shifted onto individuals who already have no time or energy to manage their own care.
The FDA draft guidance requiring interaction testing for supplements is a step forward but insufficient. The regulatory framework for dietary supplements remains fundamentally broken. The DSHEA of 1994 created a legal loophole that allows untested compounds to be sold as food. This is not science policy. It is corporate lobbying masquerading as consumer freedom
i just started taking coq10 because my doc said it helps with statin muscle pain but now i'm paranoid i'm making my cholesterol worse 😭
I used to take St. John’s wort for anxiety and didn’t tell anyone. Then I got dizzy, my heart raced, and I thought I was having a panic attack. Turns out it was serotonin syndrome. I was in the ER for 12 hours. Don’t be me.
Let me be clear: if you’re taking anything that came in a bottle labeled 'all-natural' without reading the fine print, you’re not being healthy-you’re being reckless. Your body isn’t a sandbox. It’s a chemical reactor. Treat it like one. Stop acting like your supplement is a yoga pose.
in india we use neem and turmeric for everything and no one dies. you americans are too scared of your own shadows. this is why you have so many mental health problems. your food is poison and your medicine is worse
In India, we have Ayurveda, which has been used for 5,000 years, and yet, we still have doctors who understand interactions. The problem is not the supplement-it is the lack of integration between traditional and modern medicine. Why can't we have both? Why must we choose sides?
This post is a textbook example of how fear drives engagement. You listed 12 potential interactions and didn’t mention that 99% of people never experience them. You’re not educating-you’re monetizing anxiety.
i read this at 2am and now i'm checking every pill in my cabinet. honestly tho i think the real problem is that we treat medicine like candy. if you're popping something because it's trendy or because your friend said it 'cleanses your liver'-you're not healing. you're gambling.
You say 'don’t assume natural means safe' but then you don’t say that pharmaceuticals aren’t natural either. All drugs are chemicals. All plants are chemicals. The difference is regulation. The real issue is that we trust pills more than plants because they’re expensive. That’s not logic. That’s capitalism.