This tool helps you understand the best pain relief alternatives to Toradol based on your medical history and pain needs
When you’re in severe pain - from a bad back injury, surgery, or a migraine that won’t quit - Toradol (ketorolac) can feel like a lifeline. It’s strong, fast-acting, and often used in hospitals or emergency rooms. But it’s not for everyone. And it’s not the only option. If you’ve been prescribed Toradol and are wondering what else might work just as well - or better - without the risks, you’re not alone.
Toradol is the brand name for ketorolac, a nonsteroidal anti-inflammatory drug (NSAID) used for short-term management of moderate to severe pain. It’s not meant for everyday headaches or mild aches. Doctors typically prescribe it for acute situations: after surgery, for kidney stones, or during flare-ups of severe arthritis. It works by blocking enzymes that cause inflammation and pain, and it’s stronger than over-the-counter NSAIDs like ibuprofen or naproxen.
But here’s the catch: Toradol has serious limits. It’s approved for use for only 5 days or less in adults. Why? Because long-term use raises your risk of stomach bleeding, kidney damage, and heart problems. The FDA warns against using it in people with kidney disease, ulcers, or those on blood thinners. Even healthy people can develop complications if they take it too long.
People often ask for alternatives to Toradol for three main reasons:
Some patients are switched off Toradol after just one dose because of nausea or dizziness. Others are told it’s unsafe because they’re over 65 or take aspirin daily. That’s when you need to know what else is out there.
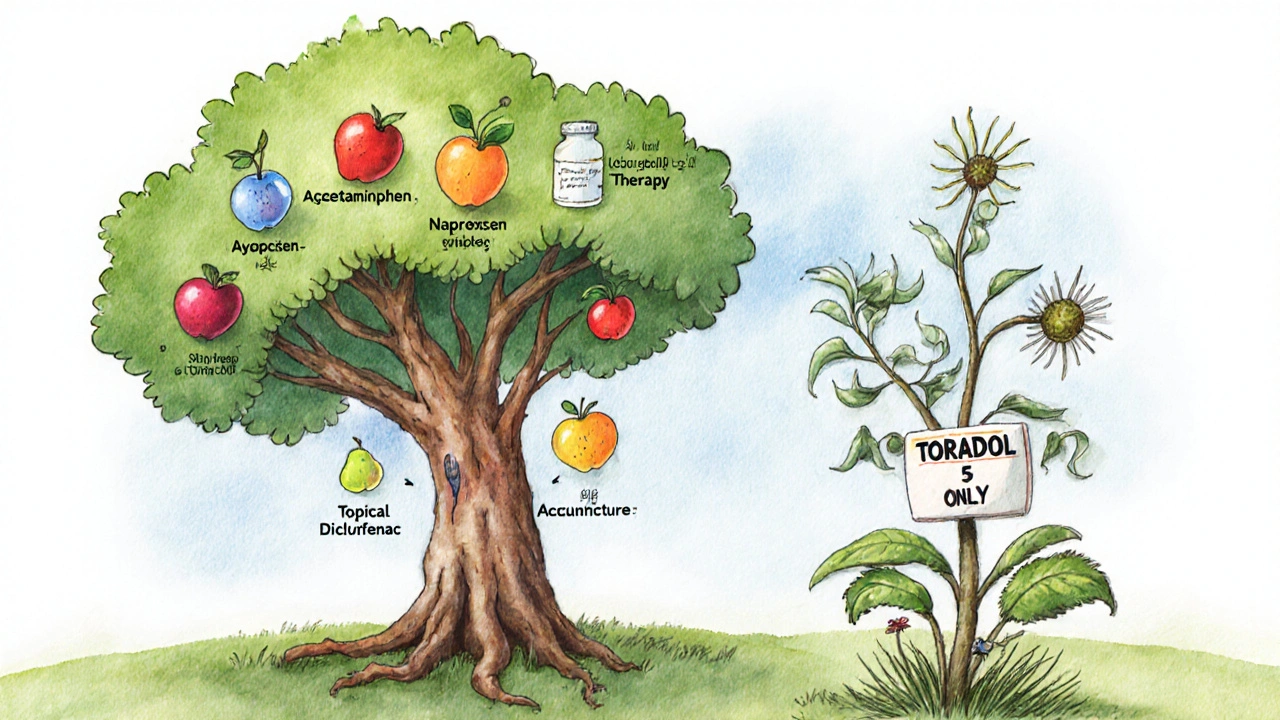
If you’re looking for something similar to Toradol but safer for longer use, oral NSAIDs are your first stop.
Ibuprofen (Advil, Motrin) is available over the counter and works well for mild to moderate pain. It’s gentler on the stomach than Toradol but still carries risks if taken daily for weeks. A typical dose is 400-800 mg every 6-8 hours.
Naproxen (Aleve, Naprosyn) lasts longer - up to 12 hours per dose - so you take it fewer times a day. Studies show it’s just as effective as Toradol for post-surgical pain, but with lower risk of ulcers when used short-term. Dose: 500 mg twice daily.
Diclofenac (Voltaren) is another option, often used for arthritis and muscle injuries. It’s available as pills, gels, or patches. The gel form lets you target pain without swallowing a pill, which helps avoid stomach issues.
All these drugs are NSAIDs, so they share the same warnings: avoid if you have kidney disease, heart failure, or a history of GI bleeding. But they’re safer than Toradol for use beyond 5 days - if taken correctly.
If you can’t take NSAIDs at all - maybe you have liver problems, or your doctor says no to anti-inflammatories - acetaminophen (Tylenol) is the go-to alternative.
It doesn’t reduce inflammation like Toradol does, but it’s very effective for pain and fever. It’s the safest choice for older adults, people with high blood pressure, or those on blood thinners. The max daily dose is 3,000-4,000 mg depending on liver health. Don’t go over it. Too much can cause serious liver damage.
Many doctors combine acetaminophen with a low-dose opioid (like tramadol) for better pain control after surgery. This combo often works better than Toradol alone, with fewer side effects.

For severe pain that NSAIDs and acetaminophen can’t touch, opioids may be necessary. But they’re not first-line options - and they’re not for long-term use.
Tramadol is a weak opioid that also affects serotonin and norepinephrine. It’s often used after dental work or minor surgeries. It’s less addictive than stronger opioids and doesn’t cause the same level of constipation or respiratory depression.
Oxycodone and hydrocodone are stronger and more effective for intense pain, like after major surgery or broken bones. But they come with big risks: drowsiness, addiction, tolerance, and withdrawal. They’re only prescribed for a few days at a time, and never without a clear plan to taper off.
Studies from the Journal of the American Medical Association show that for most acute pain, combining acetaminophen and ibuprofen gives pain relief equal to low-dose opioids - without the addiction risk. That’s why many ERs now avoid opioids unless absolutely necessary.
Medication isn’t the only way to manage pain. Sometimes, the best alternative isn’t another pill - it’s a change in approach.
These methods don’t work overnight. But if you’re dealing with pain that lasts weeks or months, they’re often more effective - and safer - than long-term NSAID use.
Here’s how Toradol stacks up against the most common alternatives:
| Option | Strength | Duration | Best For | Risks |
|---|---|---|---|---|
| Toradol (Ketorolac) | Very High | 4-6 hours | Severe acute pain (post-op, kidney stones) | Stomach bleeding, kidney damage, max 5 days |
| Naproxen | High | 12 hours | Arthritis, muscle pain, longer-term use | GI issues, heart risk with long use |
| Ibuprofen | Moderate | 6-8 hours | Mild to moderate pain, fever | Stomach upset, kidney strain with high doses |
| Acetaminophen | Moderate | 4-6 hours | Pain without inflammation, sensitive stomach | Liver damage if overdosed |
| Tramadol | Low to Moderate | 4-6 hours | Moderate to severe pain, opioid-sensitive patients | Dizziness, addiction risk, seizures |
| Topical Diclofenac Gel | Moderate | 8-12 hours | Localized pain (knees, shoulders) | Skin irritation, minimal systemic risk |
As you can see, Toradol is the strongest option - but also the riskiest. For most people, naproxen or a combo of acetaminophen and ibuprofen gives nearly the same relief with far fewer dangers.
There are clear red flags that mean you should never take Toradol:
If any of these apply to you, Toradol is not an option. Your doctor should offer safer alternatives based on your medical history.
If your doctor gives you Toradol, here’s what to do:
Many people feel better after a few days and stop calling their doctor. But pain that lasts beyond that needs a different plan - not more Toradol.
Toradol is powerful, but it’s not the answer for most long-term pain. The best alternative depends on your body, your condition, and your history. For some, it’s naproxen. For others, it’s acetaminophen with physical therapy. For severe cases, tramadol or short-term opioids might be needed - but only with careful monitoring.
The goal isn’t just to kill pain. It’s to manage it safely. The strongest drug isn’t always the best one. Sometimes, the smartest choice is the one that keeps you healthy for the long haul.
Yes, Toradol is significantly stronger than ibuprofen. It’s designed for acute, severe pain and works faster and more intensely. But ibuprofen is safer for regular use and can be just as effective for moderate pain when taken correctly. Toradol is not meant to replace daily pain relievers.
Yes, acetaminophen (Tylenol) can be safely combined with Toradol under medical supervision. Many hospitals use this combo because it reduces the amount of NSAID needed, lowering stomach and kidney risks. But never mix them without talking to your doctor first.
Naproxen is generally considered the safest NSAID for long-term use when taken at the lowest effective dose. It has a lower risk of heart problems compared to ibuprofen and diclofenac, and it lasts longer, meaning fewer doses per day. Still, even naproxen isn’t risk-free - regular check-ups with your doctor are essential.
Toradol carries a high risk of serious side effects like stomach ulcers, kidney failure, and bleeding after just a few days of use. Clinical studies show these risks spike after day 5. The FDA limits it to 5 days for this reason. If you still need pain relief after that, your doctor should switch you to a safer option.
Yes - but they’re not instant fixes. Turmeric (curcumin), ginger, and omega-3 fatty acids have anti-inflammatory effects shown in studies. Topical treatments like capsaicin cream or cold therapy can help with localized pain. Physical therapy and posture correction often reduce pain long-term without drugs. These work best alongside - not instead of - medical advice.
If you’re currently taking Toradol:
If you’ve been told you can’t take Toradol:
Pain is real. But so are the risks of the drugs we use to treat it. Choosing the right alternative isn’t about finding the strongest pill - it’s about finding the smartest one for your body.
10 Responses
Acetaminophen + ibuprofen beats Toradol every time for acute pain. No opioid risks, no GI bleeding. Simple.
It’s remarkable how many people still treat pain like a problem to be obliterated rather than a signal to be understood. Toradol suppresses symptoms, yes-but it doesn’t address root causes. For chronic musculoskeletal pain, physical therapy isn’t just an alternative-it’s the foundation. And yet, we’re conditioned to reach for the strongest pill first. The real tragedy isn’t the side effects of NSAIDs; it’s that we’ve lost the habit of listening to our bodies before we reach for chemicals. If you’re still on Toradol past day five, you’re not managing pain-you’re avoiding the conversation your body is screaming to have.
OMG I had Toradol after my C-section and it was LIFE-CHANGING-but my doc didn’t warn me about the stomach stuff. I got so dizzy I thought I was dying lol. Then I switched to naproxen and felt way better. Also, heat packs are magic. 🤍
THEY DON'T WANT YOU TO KNOW THIS-TORADOL IS A BIG PHARMA TRAP TO MAKE YOU DEPENDENT ON THEIR DRUGS! THEY KNOW NAPROXEN IS CHEAPER AND SAFER, BUT THEY PAID DOCTORS TO PUSH IT! THE FDA IS CORRUPT! THEY'VE BEEN HIDING THE TRUTH ABOUT KETOROLAC FOR DECADES!! THEY'RE USING IT TO CONTROL THE POPULATION!!
Y’all are so naive. 😒 Toradol? Please. Big Pharma’s latest cash grab. They’ll pump you full of ketorolac then slap you with a $2000 bill. Meanwhile, turmeric and acupuncture? Free. Natural. Safe. But noooooo, let’s just keep swallowing poison because the ads said so. 🤡💊 #PharmaLies
It is an incontrovertible fact that the indiscriminate use of nonsteroidal anti-inflammatory agents, particularly ketorolac, constitutes a gross negligence in contemporary clinical practice. The FDA’s five-day limit is not a suggestion-it is a legal and ethical imperative. To prescribe beyond this threshold is to violate the Hippocratic Oath. One must consider the systemic erosion of medical judgment in favor of pharmaceutical convenience. This is not medicine. It is commodification.
Based on the comparative efficacy data presented, naproxen demonstrates a superior risk-benefit profile for persistent moderate-to-severe pain states, particularly in populations with comorbid cardiovascular risk factors. The pharmacokinetic half-life advantage (12–17 hours) reduces dosing frequency, thereby improving adherence and minimizing peak-trough fluctuations in plasma concentration. Additionally, the lower incidence of gastrointestinal hemorrhage compared to diclofenac and ketorolac is statistically significant (p < 0.01 in multiple meta-analyses). It is recommended that clinicians prioritize naproxen as first-line NSAID therapy when prolonged analgesia is required.
Did you know Toradol was originally developed by the military to keep soldiers fighting through injuries? They didn’t care if they bled internally-just as long as they stayed on the front lines. Now it’s in every ER. Coincidence? I think not. 🤔
my doc gave me toradol and i felt like a superhero for 2 days then my stomach started burning and i thought i was gonna die. now im on tylenol and its like nothing. why did they even give me that stuff? its just a drug to make you feel good then wreck you. so dumb. 😭
USA made the best pain meds. Why are we letting other countries tell us what’s safe? Toradol is American strength. 🇺🇸 If you can’t handle it, maybe you shouldn’t be in pain. Chill out. 🇺🇸💪