Cumulative Drug Toxicity: How Side Effects Build Up Over Time

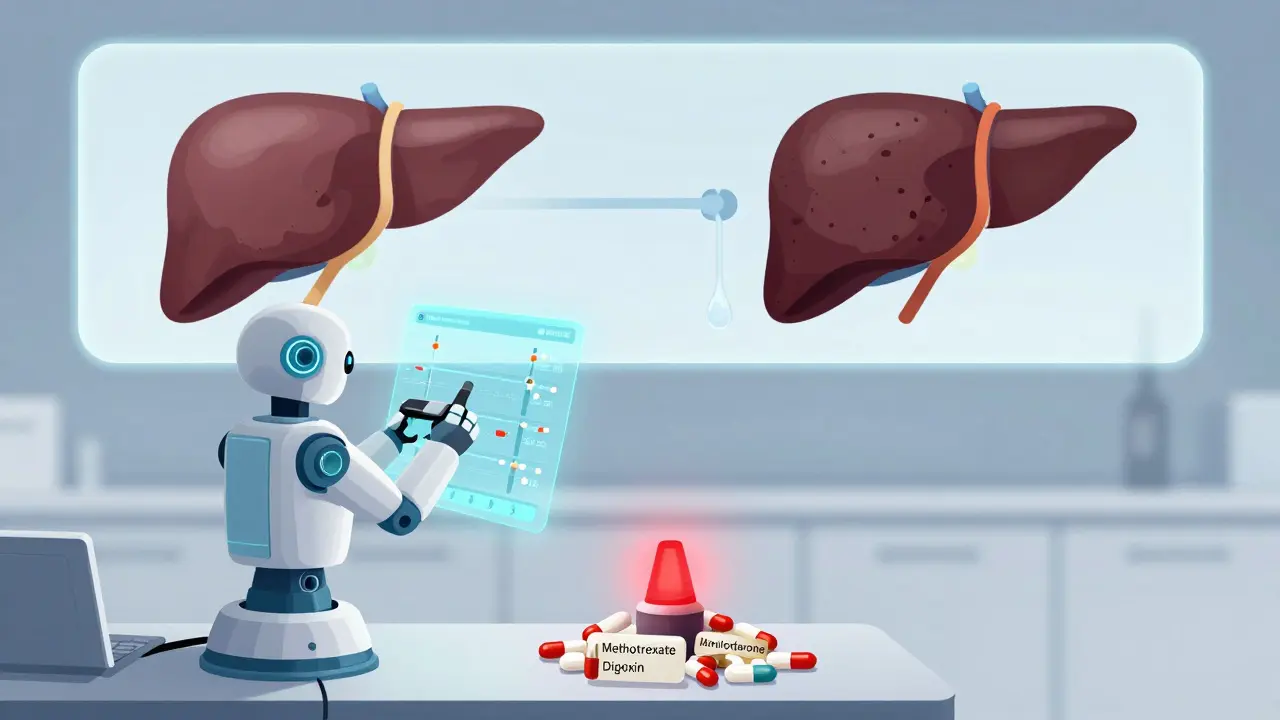
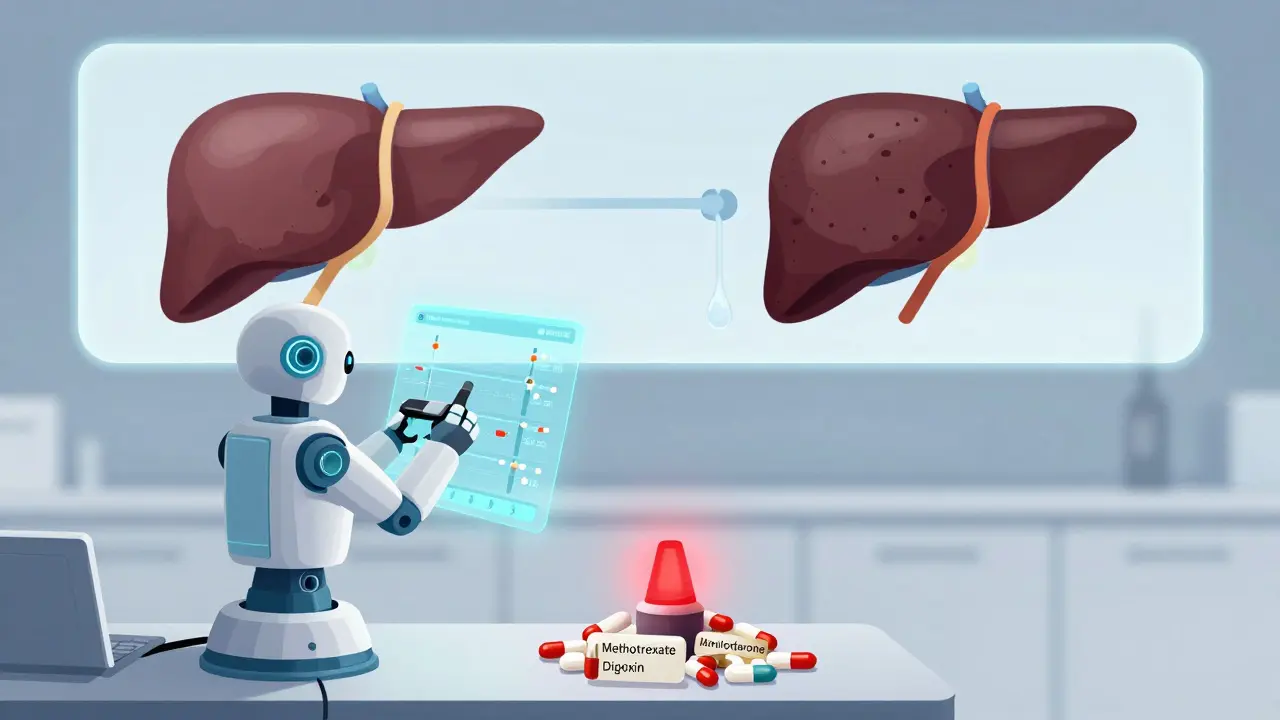
Drug Toxicity Risk Checker
Have you ever taken a medication for months or years and suddenly started feeling off-fatigued, dizzy, or nauseous-when you never had issues before? You’re not imagining it. Sometimes, the problem isn’t a new drug or a sudden mistake. It’s something quietly building up inside you: cumulative drug toxicity.
What Is Cumulative Drug Toxicity?
Cumulative drug toxicity happens when a medication stays in your body longer than it should. Instead of being broken down and flushed out, it piles up over time. Think of it like leaving a faucet running in a sink without draining it. Eventually, the water overflows. With drugs, the overflow is side effects-some mild, some dangerous.
This isn’t the same as an allergic reaction or a bad reaction after one dose. That’s acute toxicity. Cumulative toxicity creeps in slowly. You might take the same pill every day for six months, and nothing happens. Then, around month eight, you start having trouble breathing, your heart races, or your liver enzymes spike. By then, the drug concentration in your blood may have doubled-or tripled-since you started.
Drugs with long half-lives are the biggest culprits. A half-life is how long it takes for half the drug to leave your system. If a drug has a half-life of 24 hours, it takes about five days to clear. But if it’s 72 hours? That’s two weeks. Some drugs, like amiodarone (used for irregular heartbeats) or digoxin (for heart failure), have half-lives of weeks or even months. They don’t just linger-they collect.
Fat-soluble drugs are especially tricky. Vitamins A, D, E, and K, as well as heavy metals like lead and mercury, get stored in your fat and bones. Your body can’t easily get rid of them. Even if you stop taking them, they can keep leaking back into your bloodstream for years.
Who’s Most at Risk?
It’s not just older people. But they’re the most vulnerable. As we age, our livers and kidneys don’t work as well. That means drugs aren’t processed or cleared as fast. Studies show that people over 65 with reduced kidney or liver function can hold onto drugs 30-50% longer than younger adults. That’s why the American Geriatrics Society’s Beers Criteria lists 34 medications as high-risk for seniors due to cumulative buildup.
People with chronic conditions are also at higher risk. If you’re on long-term medications for high blood pressure, arthritis, depression, or cancer, you’re exposed to these drugs day after day, year after year. A 2019 study in the
Journal of the National Cancer Institute found that after six treatment cycles of targeted cancer drugs, over half of patients had experienced serious side effects-even though the first cycle showed only mild reactions.
Even people who take their meds exactly as prescribed aren’t safe. One oncologist on Reddit shared a case where a patient on amiodarone developed severe lung scarring after taking a cumulative dose of over 600 grams. All blood tests looked normal during checkups. The problem? Standard monitoring doesn’t track total lifetime exposure. It only checks current levels. By the time symptoms show up, the damage is often irreversible.
How It Builds: Real Numbers, Real Consequences
Let’s look at the data. In cancer treatment, the risk of severe side effects isn’t linear. It’s exponential. The same study found that if a patient had a 25% chance of side effects in the first cycle, by the sixth cycle, their risk jumped to nearly 66%. That’s not a fluke. It’s the math of accumulation.
Take methotrexate, a drug used for rheumatoid arthritis and some cancers. A 2021 study showed that when clinics started tracking the total lifetime dose, adverse events dropped by 37%. That’s not magic. It’s awareness. Once doctors knew how much the patient had taken over years, they could adjust before damage occurred.
Even antibiotics aren’t safe. The CDC now tracks cumulative antibiotic exposure to prevent resistance and organ damage. Long-term use of certain antibiotics like gentamicin can cause permanent hearing loss or kidney damage-not from one dose, but from months of daily use.
The FDA’s adverse event database recorded over 12,000 cases of cumulative toxicity between 2018 and 2022. Nearly half involved blood thinners like warfarin. Another 28% involved heart meds. These aren’t rare events. They’re predictable-and preventable.

Why Doctors Miss It
You’d think doctors would catch this. But they often don’t. Here’s why:
- Most electronic health records don’t automatically add up your total drug dose over time.
- Doctors focus on current symptoms, not lifetime exposure.
- Many drugs don’t have clear cumulative dose limits on their labels.
- Patients don’t know to mention how long they’ve been on a drug-they just say, “I’ve been taking this for years.”
A 2022 Medscape survey found that 67% of doctors had seen at least one case of serious cumulative toxicity in the past year. But 82% said patients didn’t follow up with monitoring. Why? Because no one told them it was a problem.
Nurses on AllNurses forums report the same thing: patients are confused. “I’ve taken this for five years and never had issues,” they say. “Why now?” The answer: because the drug finally reached the tipping point.
How to Protect Yourself
You can’t control how your body processes drugs. But you can control your awareness. Here’s what to do:
- Know your meds. Ask your pharmacist or doctor: “Is this drug known to build up in the body? Is there a lifetime limit?”
- Track your doses. Keep a simple log: drug name, dose, start date. Apps like Medisafe or even a notes app on your phone work.
- Ask for monitoring. If you’re on digoxin, lithium, amiodarone, or methotrexate, request periodic blood tests-not just for current levels, but for trends over time.
- Speak up about new symptoms. Don’t assume fatigue, tingling, or memory lapses are just aging. Ask: “Could this be from a drug I’ve been taking for years?”
- Review your list yearly. Ask your doctor: “Which of these meds are still necessary? Could any be stopped or switched?” Polypharmacy is a major risk factor.
What’s Changing in Medicine
Good news: the system is waking up.
In 2024, the European Medicines Agency made cumulative toxicity assessments mandatory for all new drugs meant for long-term use. The FDA now requires cumulative dose warnings on 78% of new cancer drugs-up from just 52% in 2017.
Pharmacies are starting to track total doses. A 2023 study showed that pharmacist-led monitoring cut hospital admissions for drug toxicity by 29% across 45 health systems.
And technology is catching up. AI models at Memorial Sloan Kettering can now predict your personal risk of toxicity by analyzing 27 factors: your age, kidney function, other meds, genetics, even your diet. Early results show 82% accuracy.
The global market for therapeutic drug monitoring is expected to hit $4.7 billion by 2028. That’s because more people are realizing: we’ve been treating symptoms, not causes. Cumulative toxicity isn’t an accident. It’s a system failure.
Bottom Line: It’s Not Just About the Dose. It’s About the Time.
Medication isn’t harmless just because it’s prescribed. Some drugs are like slow-burning fires. They don’t explode on day one. They smolder. And when they finally catch, the damage is deep.
If you’re on a long-term medication, especially if you’re over 50 or have kidney or liver issues, don’t wait for symptoms to appear. Ask your doctor: “What’s my total dose so far? Is there a limit I should know about?”
Your body remembers every pill. Make sure your doctor does too.
Can cumulative drug toxicity be reversed?
Sometimes, yes-but not always. If caught early, stopping the drug and supporting your liver and kidneys with hydration and nutrition can help your body clear the buildup. But if the toxicity has caused permanent damage-like lung scarring from amiodarone, hearing loss from gentamicin, or heart muscle damage from doxorubicin-that damage is often irreversible. Early detection is critical.
Are over-the-counter drugs capable of cumulative toxicity?
Absolutely. Acetaminophen (Tylenol) is the leading cause of acute liver failure in the U.S., but chronic overuse-even just a few extra pills a day over months-can cause slow, silent liver damage. Herbal supplements like kava and comfrey, and even high-dose vitamin A or D, can build up and cause toxicity. Just because it’s sold without a prescription doesn’t mean it’s safe for long-term use.
How do I know if my medication has a cumulative dose limit?
Check the drug’s prescribing information, usually available on the manufacturer’s website or through your pharmacist. Drugs like doxorubicin (maximum 450 mg/m² lifetime), amiodarone (monitor for lung/liver toxicity after 6 months), and lithium (long-term kidney risk) have well-documented limits. If you’re unsure, ask your pharmacist to check the FDA-approved label for phrases like “cumulative dose,” “lifetime exposure,” or “toxicity risk with prolonged use.”
Why don’t all doctors track cumulative doses?
Many electronic health records don’t calculate total lifetime doses automatically. Doctors are under time pressure and focus on immediate concerns. Also, not all drugs have clear, evidence-based cumulative limits. Until recently, the medical system didn’t prioritize this type of tracking. But that’s changing-especially in oncology, cardiology, and rheumatology, where the stakes are highest.
Can lifestyle factors make cumulative toxicity worse?
Yes. Alcohol, smoking, and certain foods can strain your liver and kidneys, slowing drug clearance. Dehydration reduces kidney function. Obesity increases fat storage for fat-soluble drugs. Even environmental toxins-like lead in old pipes or mercury in fish-can add to your body’s total toxic load. If you’re on long-term meds, minimizing these stressors helps your body manage the drugs better.
If you’ve been on the same medication for years, don’t assume it’s safe just because you feel fine. The body doesn’t always warn you before it breaks down. Stay informed. Stay proactive. Your future self will thank you.


8 Responses
This is the exact kind of systemic negligence that gets people killed. We're not talking about minor side effects here-we're talking about iatrogenic catastrophes masked as "normal aging." The FDA's database shows over 12,000 cases in five years, and yet no mandatory cumulative dosing alerts in EHRs? That's not incompetence-it's institutional malpractice. Pharmacies track prescriptions, but not total lifetime exposure? That's like monitoring your car's fuel level but ignoring how many gallons you've burned since 2010. Someone's getting rich off this slow-motion poisoning, and it's not the patients.
And don't get me started on "over-the-counter" drugs. Tylenol isn't "safe"-it's a silent hepatic assassin. People pop four a day for migraines and wonder why their liver enzymes are through the roof. No one warns them. No one checks. No one cares until the transplant list is the only option left.
Stop calling this "risk." Call it what it is: predatory pharmacology enabled by bureaucratic apathy.
And if your doctor says "it's fine," ask them how many patients they've lost to cumulative toxicity. I dare you.
It’s fascinating how the biomedical paradigm remains so fundamentally reductionist-focusing on pharmacokinetic parameters in isolation rather than adopting a systems biology approach to polypharmacological burden. The notion that we can discretely evaluate drug exposure without accounting for epigenetic modulation, mitochondrial dysfunction, or gut microbiome-mediated metabolic interference is not merely archaic-it’s epistemologically bankrupt.
Consider the case of amiodarone: its lipophilicity and half-life are well-documented, yet clinical guidelines still treat it as a binary yes/no prescription rather than a dynamic, cumulative bioaccumulative stressor. The failure to integrate longitudinal biomarker trajectories-say, serial KL-6 for pulmonary toxicity or serum thyroglobulin for thyroid dysfunction-is a glaring lacuna in translational medicine.
Until we reframe toxicity not as an event but as a trajectory, we’ll continue to treat symptoms while the substrate of disease silently proliferates. The EMA’s 2024 mandate is a start, but it’s still tethered to a mechanistic worldview that ignores emergent systemic collapse.
Let me be perfectly clear: this is not just a medical issue-it’s a moral crisis. We have entrusted our bodies to a system that treats human beings as data points, not living, breathing organisms with finite capacity for detoxification. Every pill you take, every daily dose, every prescription renewed without review-it’s a silent debt your liver, kidneys, and nervous system are paying in real time.
And yet, we celebrate innovation in drug development while ignoring the most basic principle of stewardship: do no harm over time. We’ve optimized for short-term efficacy and profit margins, and in doing so, we’ve created a generation of patients who are slowly being poisoned by the very things meant to heal them.
But here’s the hope: awareness is the first step. Tracking your doses isn’t just responsible-it’s revolutionary. When you start asking, "What’s my total?" you’re not just protecting yourself-you’re challenging a broken system. You’re saying: I am not a statistic. I am not collateral damage. I am a person who deserves to live, not just survive.
And if your doctor can’t answer that question? Find one who can. Your life depends on it.
This isn’t fearmongering. This is medicine, finally waking up.
ok so like… i’ve been on lithium for 12 years and never thought about this?? like i just thought "oh it’s fine i take it every day" but now i’m like… wait… is my brain just… full of lithium?? like literally??
and i read that amiodarone thing and now i’m scared to even look at my meds list because what if i’ve been slowly poisoning myself and no one told me??
also my cousin died of liver failure from tylenol and they said she "overdosed" but she only took 4 a day for 3 years?? like… that’s not an overdose… that’s a system failure.
why does no one talk about this?? why is this not on every med bottle??
also i think i just had a panic attack.
pls help.
ps: i’m gonna start a notes app. i swear. i’m gonna track every damn pill.
pps: typo. i meant to say "i’m gonna track every damn pill" but i’m already typing too fast because i’m scared.
ppps: is this comment too emotional? i don’t care. i need someone to say this out loud.
I’ve been on methotrexate for RA for seven years. I started having tingling in my hands last year. My rheumatologist said "it’s probably nerve compression from arthritis." I didn’t push back because I trusted him. Then I found this post.
I checked my records. I’ve taken over 1,200 doses. No one ever told me there was a lifetime cap. No one asked me how long I’d been on it. No one tracked trends. Just "lab numbers today."
I went back yesterday. I asked for cumulative dose history. He looked confused. Then he pulled up the chart. Silence. Then he said, "We should’ve been monitoring this more closely. I’m sorry."
I cried in the parking lot.
This isn’t just about science. It’s about being seen. It’s about being listened to. It’s about not being dismissed as "just aging."
If you’re on long-term meds-please, please, please ask. Even if they look at you weird. Even if they say "it’s not necessary." Ask anyway. Your body is trying to tell you something.
You’re not crazy. You’re not exaggerating. You’re just overdue for someone to finally pay attention.
lol so now we’re blaming doctors for not doing math? take a pill, get sick, blame the system. newsflash: your body isn’t a calculator. if you feel weird, stop taking it. problem solved.
also tylenol kills? shocker. next you’ll say water is toxic if you drink too much.
everyone’s just scared of medicine now. chill out. your meds aren’t slowly murdering you. you’re just anxious.
and no, i don’t track my doses. i’m not a robot.
Thank you for this profoundly necessary piece. As a clinician with over two decades of experience in chronic disease management, I can confirm: cumulative toxicity is the silent epidemic of modern pharmacotherapy. We are trained to treat acute events, not chronic accumulation. Our systems are not designed for longitudinal care.
But here’s what we can do: First, we must normalize the question: "How long have you been taking this?" Second, we must integrate cumulative dosing into electronic health records as a mandatory field-not an optional note. Third, we must empower patients with accessible, real-time tools to track exposure, as you’ve outlined.
I’ve seen patients recover fully when caught early-liver enzymes normalize, neuropathy regresses, cognitive fog lifts. But I’ve also seen irreversible damage. The difference? Timing. Awareness. Advocacy.
To the patient who wrote about their lithium: You are not alone. Your fear is valid. Your voice matters. And your request for a cumulative dose review is not just appropriate-it is essential. I would be honored to help you navigate this.
Let us not wait for the next tragedy. Let us begin now-with curiosity, with courage, with compassion.
Thank you for writing this. I am from India, and here, most people take antibiotics for every little cough or fever-without prescription, without follow-up. I’ve seen elderly relatives on beta-blockers for 15 years, never checked for kidney function. No one knows what "half-life" means. The pharmacy guy just hands them the pill.
This post is not just informative-it’s a lifeline.
I’ve started sharing it with my family. My mother is on amiodarone. I just called her doctor and asked for her total cumulative dose. He didn’t know. He said he’d check.
That’s the first step.
And if you’re reading this, and you’ve been on the same pill for five years…
…ask.
Just ask.
It might save your life.
With deep respect,
Vinaypriy