For many heart patients, digoxin is a quiet but powerful part of their daily routine. It’s not new-it’s been around since the 1930s-and it’s not flashy like the latest heart drugs. But for some people, especially those with heart failure or atrial fibrillation, it still makes a real difference. The problem? Digoxin doesn’t play well with others. Even small changes in what you take, eat, or drink can push it from healing to dangerous. If you’re on digoxin, you’re not just managing a heart condition-you’re managing a minefield of interactions.
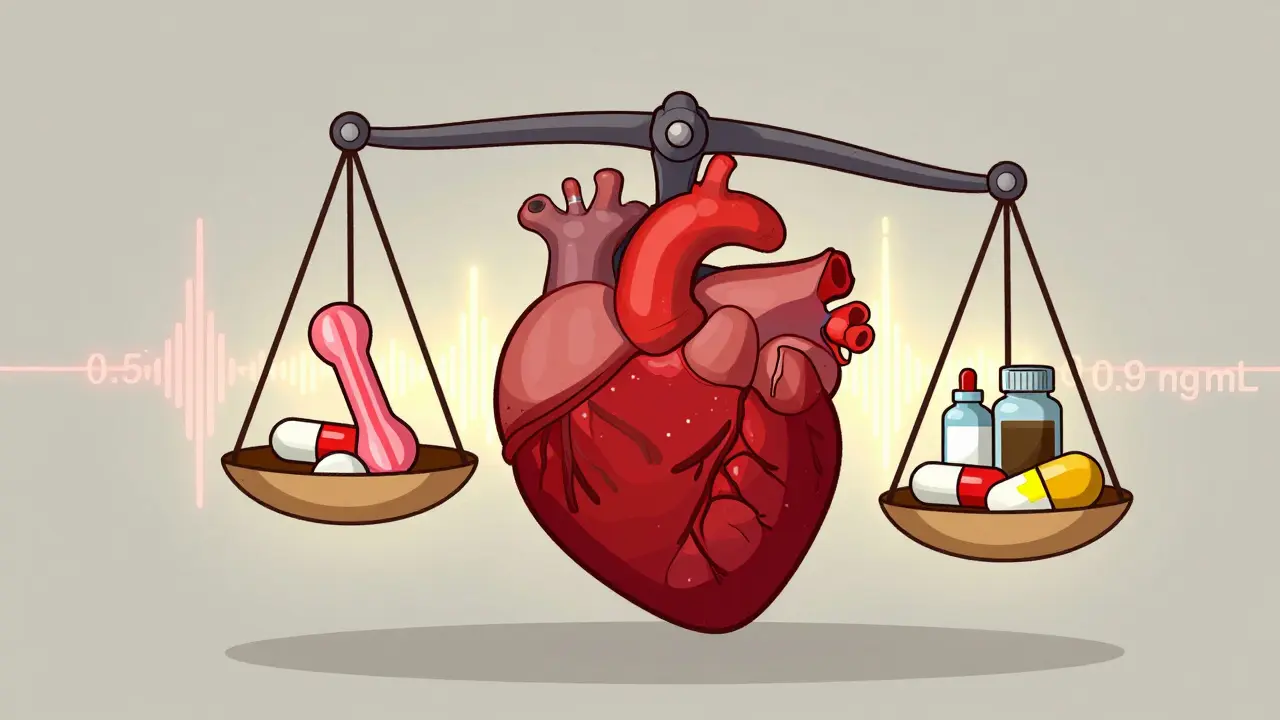
Digoxin works by making your heart beat stronger and more regularly. It’s taken from the foxglove plant, and while that sounds natural, it’s anything but gentle. The dose that helps you is almost the same dose that can hurt you. Doctors call this a narrow therapeutic index. That means your blood level needs to stay between 0.5 and 0.9 ng/mL. Go above 2.0 ng/mL, and you’re in toxicity territory. And here’s the scary part: you can hit that level even if you’re taking your exact prescribed dose.
Why? Because other things change how your body handles digoxin. Some drugs make it build up. Others make it disappear. Some foods block it. And your kidneys? If they’re not working perfectly-which is common in older heart patients-digoxin sticks around longer. That’s why people over 65, especially those with kidney issues or low body weight, are at much higher risk.
Not all drug interactions are created equal. Some are mild. Digoxin’s are not. Here are the five most dangerous ones you need to watch for:
Digoxin doesn’t just react with pills. It reacts with your breakfast.
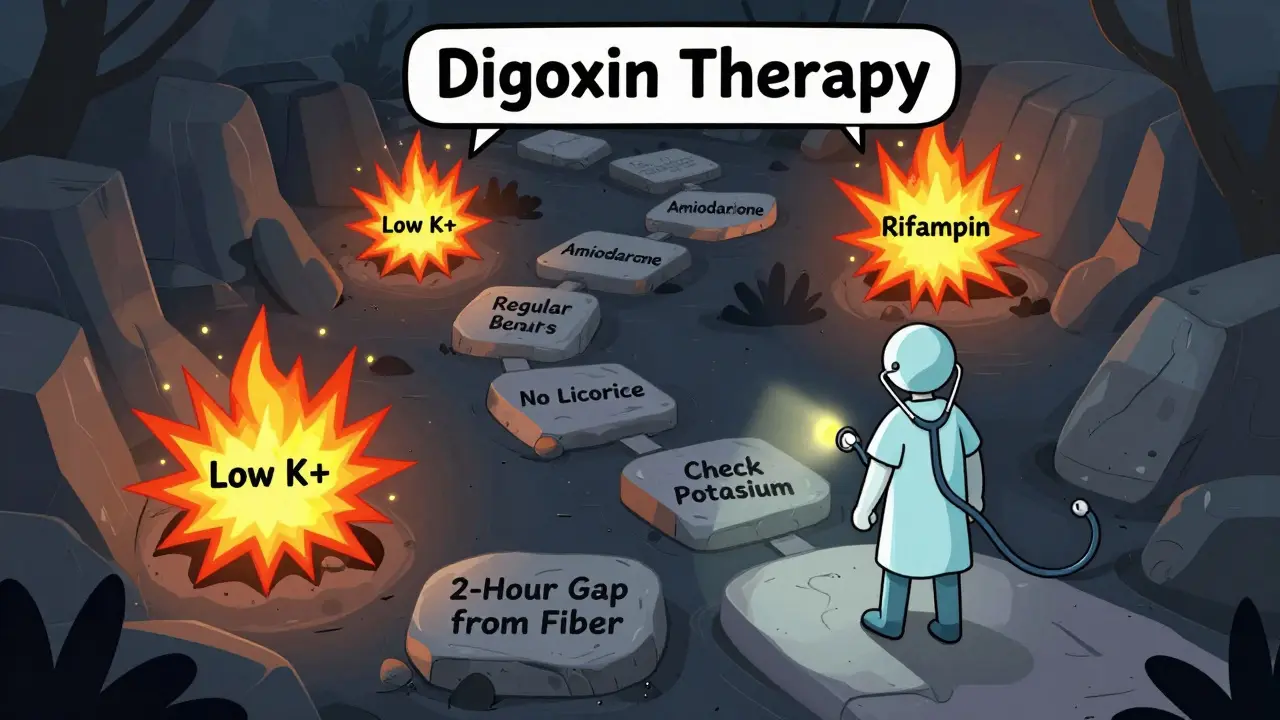
High-fiber foods like oatmeal, bran cereal, and psyllium fiber supplements can block digoxin from being absorbed. One study showed absorption dropped by 20-30% when taken with oatmeal. That means your dose isn’t working. The fix? Take digoxin at least two hours before or after eating these foods. One Reddit user said switching from taking digoxin with breakfast to taking it two hours before solved their low levels.
Black licorice is another silent danger. It contains glycyrrhizin, which lowers potassium. And low potassium is one of the biggest triggers for digoxin toxicity. Even a small amount-like a few pieces of candy a week-can push you over the edge. The Heart and Stroke Foundation of Canada warns: no black licorice, ever, if you’re on digoxin.
And don’t forget antacids. Those Tums or Maalox you take for heartburn? They contain aluminum or magnesium, which bind to digoxin in your gut and stop it from being absorbed. One Mayo Clinic study found that 22% of digoxin-related ER visits were linked to over-the-counter antacids. If you need antacids, take them at least two hours after your digoxin.
Some interactions are less obvious but just as dangerous:
If you’re on digoxin, you need a plan-not just a prescription.
Not everyone on digoxin is equally vulnerable. The American College of Cardiology created a simple risk score in 2023 to help doctors spot who’s in danger:
If your score is 5 or higher, you’re high risk. You need weekly blood tests and close monitoring. If you’re over 75, have kidney problems, and take digoxin with diltiazem? You’re likely in that group. Don’t assume you’re fine just because you’ve been on it for years.
Digoxin prescriptions have dropped by 38% since 2010. Newer drugs like SGLT2 inhibitors and ARNIs are safer and more effective for most people. But digoxin still has a place. It’s cheap-$4 to $6 a month. It helps with symptoms like fatigue and shortness of breath when other meds aren’t enough. And for older patients with persistent atrial fibrillation, it’s still a go-to for controlling heart rate.
The key isn’t to avoid it entirely. It’s to use it wisely-with eyes wide open. If you’re on digoxin, you’re not just taking a pill. You’re managing a delicate balance. One wrong interaction, one missed potassium test, one piece of licorice-and things can go wrong fast.
But if you know the risks, check your levels, and talk to your doctor about every new medicine or supplement, you can stay safe. Digoxin isn’t going away. And for many, it still works. Just don’t let it catch you off guard.
No. High-fiber foods like oatmeal, bran, and psyllium can reduce digoxin absorption by 20-30%. Take digoxin at least two hours before eating these foods. Many patients see their digoxin levels stabilize after making this simple change.
Yes. Black licorice contains glycyrrhizin, which lowers potassium levels. Low potassium dramatically increases the risk of digoxin toxicity-even if your digoxin level is normal. Avoid all black licorice, including candy, tea, and supplements. Red licorice is safe, as it doesn’t contain glycyrrhizin.
Every 3-6 months if you’re stable and not starting new meds. But if you begin a new drug like amiodarone, diltiazem, or rifampin-or if you have kidney issues, are over 75, or feel unwell-get tested weekly for at least two weeks. Your doctor should adjust testing based on your risk score.
No. Stopping digoxin suddenly can cause your heart failure or atrial fibrillation to worsen. Always talk to your doctor before making any changes. Even if you feel fine, your body may still need it. Your symptoms don’t always match your blood levels.
If you miss a dose and remember within 12 hours, take it right away. If it’s been more than 12 hours, skip the missed dose and take your next one at the regular time. Never double up. Taking too much can be life-threatening.
Yes. The DIG-FAST trial is testing a new extended-release digoxin formula that reduces peak-trough fluctuations by 30%, which could lower interaction risks. Results are expected in mid-2024. But for now, the focus is on safer use of existing digoxin-not replacing it.
9 Responses
Digoxin is such a weird drug. I’ve been on it for 5 years and never knew oatmeal could mess with it. I take mine with breakfast every day. Guess I’m switching to taking it before I eat now.
Black licorice??? 😱 I had a bag of it last week… I’m so done. No more candy for me. Thanks for the wake-up call!! 🙏❤️
This article is 90% common sense. Why are people still getting poisoned by digoxin? It’s not rocket science. Stop eating fiber with your meds. Stop taking licorice. Get your potassium checked. Done.
As a clinical toxicologist, I’ve seen multiple cases of digoxin toxicity secondary to unrecognized drug interactions-particularly with amiodarone and diltiazem. The narrow therapeutic window demands vigilant monitoring. Serum levels alone are insufficient; clinical context, renal function, and electrolyte status must be integrated. I strongly recommend automated alerts in EHRs for concurrent prescribing of high-risk agents. Patient education is critical, but system-level safeguards are non-negotiable.
So let me get this straight… I can’t have licorice, oatmeal, antacids, supplements, or friends who give me herbal tea… but I can still take a pill made from a poisonous plant? 🤡 I feel like I’m in a medical horror movie.
It’s fascinating how a drug from a flower can hold so much power-and so much danger. We treat medicine like it’s a simple switch, but the body is a symphony. One wrong note, and everything collapses. Digoxin reminds us that even the oldest tools can be the most delicate. We need humility, not just dosage charts.
If digoxin levels are so unstable, why isn’t there a better way to monitor them in real time? Like a wearable that tracks serum concentration? We have glucose monitors for diabetics-why not digoxin? The technology exists. The will doesn’t.
It’s unacceptable that in the 21st century, patients are still being poisoned by a 90-year-old drug because doctors don’t educate properly. In the UK, we’ve had guidelines for this since the 1990s. American healthcare is dangerously lax. This isn’t just negligence-it’s systemic failure.
I live in India and my doctor gave me digoxin without even asking about my diet. No one told me about licorice or fiber. People here just take pills and hope. This info should be in every language. Not just English.