
When you hear about GLP-1 agonists, you might think of diabetes. But today, these drugs are being used for something else entirely: weight loss. Medications like Wegovy, Ozempic, and Zepbound are helping people lose 10%, 15%, even 20% of their body weight-numbers that used to require surgery. But they’re not magic pills. They come with real side effects, high costs, and long-term questions. If you’re considering one, you need to know what you’re signing up for.
GLP-1 agonists mimic a hormone your body already makes after eating. This hormone, called glucagon-like peptide-1, tells your brain you’re full and slows down how fast your stomach empties. The result? You eat less without feeling hungry all the time.
Unlike diets that rely on willpower, these drugs change your biology. They act on the hypothalamus-the part of your brain that controls appetite-and turn down the signals that make you crave food. At the same time, they delay digestion. That’s why you feel full longer after meals, even small ones.
They also help your pancreas release more insulin when your blood sugar rises, and reduce the liver’s production of glucose. That’s why they were first approved for type 2 diabetes. But the weight loss? That’s the side effect everyone noticed-and started asking for.
Real numbers matter here. In clinical trials, people using semaglutide (Wegovy) lost an average of 15.8% of their body weight over 68 weeks. That’s not a few pounds-it’s 30, 40, even 60 pounds for many. Tirzepatide (Zepbound) did even better: 20.9% weight loss in the same timeframe. For comparison, older weight loss drugs like phentermine-topiramate or orlistat typically deliver 5-10% loss.
What does that look like in real life? One user on Reddit lost 78 pounds in 10 months on Wegovy. Another said they cut their portion sizes in half without feeling deprived-something no diet had ever done for them.
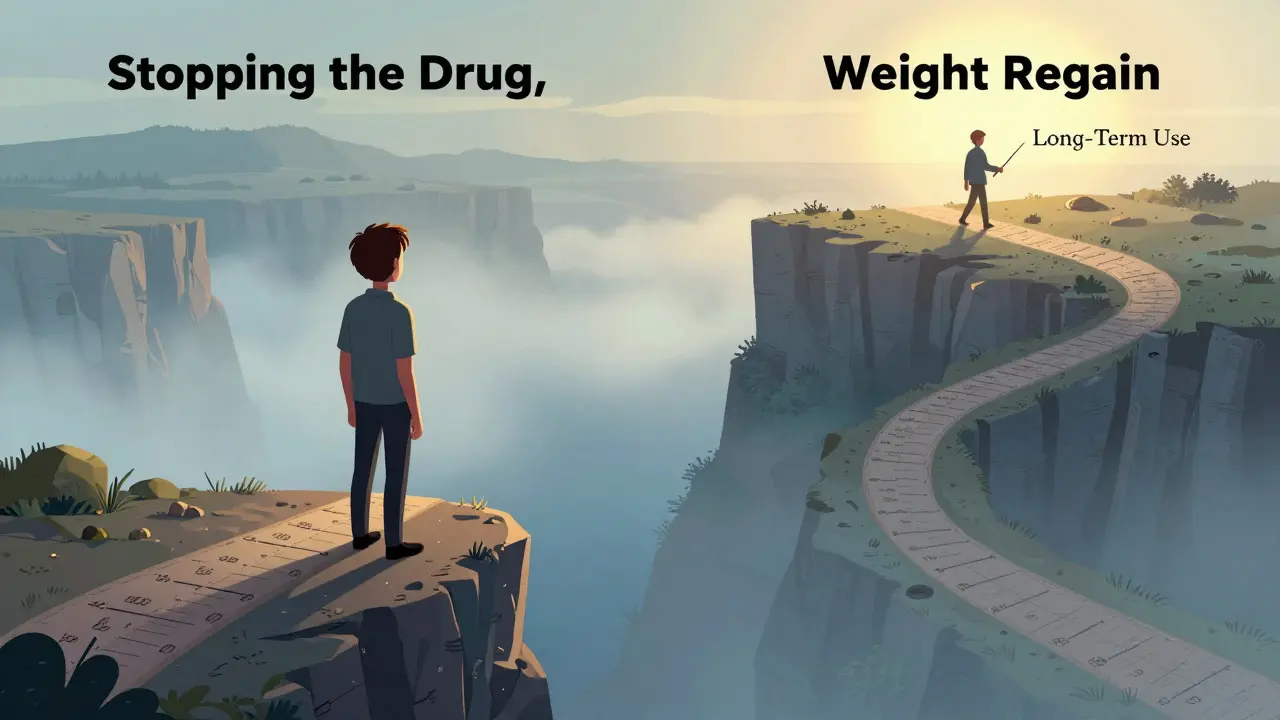
But here’s the catch: these results only happen if you keep taking the drug. When people stop, they regain 50-70% of the weight within a year. That’s not a failure-it’s how the drugs work. They don’t fix your metabolism. They manage it. Think of them like blood pressure medication: you need to keep taking them to keep the benefit.
If you’ve seen social media posts about GLP-1 agonists, you’ve probably heard about nausea. And yes-it’s common. Between 70% and 80% of users experience it, especially in the first few weeks. About 30-40% say it’s moderate to severe. But here’s what most people don’t tell you: it usually gets better.
After 8-12 weeks, most side effects fade. Diarrhea, vomiting, and stomach pain also drop off significantly. The key is slow titration. Starting at 0.25 mg weekly and increasing every four weeks gives your body time to adjust. Jumping straight to the full dose? That’s how people end up quitting.
Other side effects include dizziness, fatigue, and constipation. A small number report hair loss, though it’s unclear if that’s directly caused by the drug or by rapid weight loss itself. The biggest concern for doctors is gallbladder problems-like gallstones-which can increase with fast weight loss.
There’s also a black box warning from the FDA about thyroid tumors in rodents. No human cases have been confirmed, but if you or a family member has a history of medullary thyroid cancer or multiple endocrine neoplasia, you shouldn’t take these drugs.

Wegovy costs about $1,349 a month without insurance. Ozempic (the same drug, but approved for diabetes) is cheaper at $936, but it’s not legally prescribed for weight loss unless your doctor can justify it. Tirzepatide (Zepbound) is priced similarly.
Insurance coverage is a nightmare. Only 37% of private plans in the U.S. cover Wegovy for obesity as of 2023. Even if you have a BMI over 30 and diabetes or high blood pressure, your insurer might still deny it. Many patients are forced to pay out-of-pocket or switch to cheaper, less effective options.
Some people try to stretch their supply by splitting doses or using expired pens. That’s dangerous. These are precision medications. Dosing too low won’t help. Dosing too high increases side effects without adding benefit.
| Medication | Weight Loss (Avg.) | Dosing | Cost (Monthly) | Key Risks |
|---|---|---|---|---|
| Wegovy (semaglutide) | 15.8% | Weekly injection | $1,349 | Nausea, vomiting, gallbladder issues |
| Zepbound (tirzepatide) | 20.9% | Weekly injection | $1,350+ | Same as Wegovy, higher GI side effects |
| Saxenda (liraglutide) | 6.4% | Daily injection | $1,200 | Nausea, pancreatitis risk |
| Qsymia (phentermine-topiramate) | 7-10% | Daily pill | $150-200 | Cognitive fog, birth defects, increased heart rate |
| Xenical (orlistat) | 5-10% | Daily pill | $100-150 | Oily stools, fecal urgency, vitamin deficiencies |
GLP-1 agonists are the only class that combines strong weight loss with proven heart benefits. Semaglutide reduced heart attacks and strokes by 26% in people with existing heart disease. No other weight loss drug has that record. But they’re also the most expensive and require injections. Pills like Qsymia or Xenical are cheaper and easier to take-but they’re less effective and come with their own problems.
These drugs aren’t for everyone. The Endocrine Society recommends them for adults with a BMI of 30 or higher, or 27 or higher with at least one weight-related condition like high blood pressure, type 2 diabetes, or sleep apnea.
They’re not for people with a personal or family history of medullary thyroid cancer. Pregnant women shouldn’t take them-there’s not enough safety data. People with a history of pancreatitis should avoid them too.
They’re also not a substitute for lifestyle changes. The best results come when people combine the drug with modest calorie reduction (500 calories less per day) and regular movement. One study showed people who added just 150 minutes of walking per week lost 30% more weight than those who only took the drug.
This is the question no one wants to ask out loud. What if you lose 50 pounds on Wegovy, and then your insurance drops coverage? Or you can’t afford it anymore?
The data is clear: 50-70% of the weight comes back within a year. That’s not weakness. It’s biology. Your body is trying to return to its old set point. The drug was holding it back. When you stop, the hunger signals come roaring back.
That’s why experts say these are long-term medications-not quick fixes. If you’re going to start one, you need to plan for the long haul. That means financial planning, mental readiness, and a support system. It’s not just about the needle-it’s about building a life you can maintain.
Right now, you need to inject these drugs. But that’s changing. Novo Nordisk is testing an oral version of semaglutide for weight loss, with results expected in 2024. Pfizer is developing danuglipron, another oral GLP-1 agonist in phase 2 trials.
If they work, they could change everything. No more needles. Lower cost. Wider access. But they’ll still have the same side effects-and the same need for long-term use.
Meanwhile, more insurance companies are starting to cover these drugs for obesity, not just diabetes. The market is projected to hit $100 billion by 2030. That means more competition, more pressure to lower prices, and more options for patients.
But for now, the choice is simple: pay $1,300 a month, deal with nausea for a few months, and hope your insurance doesn’t drop you-or accept that you might not be able to afford the treatment that could change your health forever.
Yes, for most people. Diet and exercise alone typically lead to 5-10% weight loss over a year. GLP-1 agonists like Wegovy and Zepbound deliver 15-20% loss on average. That’s not because they replace healthy habits-they enhance them. People who combine the drug with modest calorie reduction and regular activity lose significantly more than those who only take the medication.
Yes, and in fact, they’re now recommended as first-line treatment for type 2 diabetes in people with obesity or heart disease. Drugs like Ozempic and Mounjaro improve blood sugar control while helping you lose weight. Many doctors now prescribe them for both conditions at once.
They’re the same drug-semaglutide-but approved for different uses. Wegovy is FDA-approved specifically for weight loss and is marketed at a higher dose (2.4 mg). Ozempic is approved for diabetes and sold at lower doses (0.5-1 mg). Insurance often covers Ozempic for diabetes but not Wegovy for weight loss. That’s why some doctors prescribe Ozempic off-label for weight loss-it’s cheaper and sometimes easier to get covered.
So far, yes. Studies show people have safely used semaglutide for over five years with no new safety signals emerging. The biggest risks are gastrointestinal side effects early on and gallbladder issues with rapid weight loss. Long-term studies are ongoing, but current data supports continued use for weight maintenance. Stopping the drug is riskier than continuing it.
You’re likely a good candidate if your BMI is 30 or higher, or 27 or higher with a weight-related health issue like high blood pressure, diabetes, or sleep apnea. You should not take them if you or a close family member has medullary thyroid cancer or multiple endocrine neoplasia type 2. Talk to your doctor about your medical history, current medications, and whether you’re ready for long-term treatment.
To keep the weight off, yes. Like blood pressure or cholesterol medication, GLP-1 agonists manage a chronic condition. When you stop, your body tends to return to its previous weight. That doesn’t mean you’re addicted-it means your biology is working against you. Many people stay on them for years. The goal isn’t to stop-it’s to find a sustainable way to keep them in your life.
13 Responses
So I lost 40 lbs on Wegovy and now my jeans fit like they did in college. But the nausea? Oh man. First two weeks felt like I was on a pirate ship in a hurricane. Took it slow, now it’s fine. Worth it.
They call it a magic pill. I call it a very expensive way to make your stomach hate you. But hey, if you’ve got the cash and the will to endure 8 weeks of misery, more power to you.
I’m on Zepbound and honestly the biggest win isn’t the weight loss it’s that I stopped thinking about food all the time. Like, I used to plan meals like they were military operations. Now I eat when I’m hungry and stop when I’m not. Revolutionary.
It’s not about the drug. It’s about what the drug lets you do. If you take this and go back to eating like you’re on a food challenge, you’ll gain it all back. But if you use it to reset your relationship with food? That’s the real win. The needle just gives you breathing room to rebuild.
People act like this is a breakthrough. It’s not. We’ve had appetite suppressants for decades. The only difference is now they’re priced like luxury watches and marketed as ‘weight loss revolution.’ Same old biology, new markup. Also, 20% weight loss sounds great until you realize 70% of it comes back when you stop. Congrats, you just bought a subscription.
Honestly if you’re taking this because you can’t be bothered to eat salad and walk 30 minutes a day, maybe you’re not ready for this. It’s not a shortcut, it’s a tool for people who’ve already tried everything else and still can’t break the cycle. And yes, it’s expensive. Life’s expensive when you wait until you’re 200 lbs to care.
Why do people think they deserve to lose weight with a pill? I’ve been working out since I was 14. No drugs. No excuses. You want results? Earn them. This is just another way for Big Pharma to profit off people’s laziness and desperation.
My doctor put me on Wegovy after I had a pre-diabetes scare. Lost 35 lbs in 6 months. My A1c dropped from 6.1 to 5.3. I still take it. Not because I’m addicted to the drug, but because I’m addicted to feeling healthy. And I’m not stopping anytime soon.
Interesting how the article mentions thyroid tumors in rodents but dismisses it as irrelevant. Yet no one talks about the 30% increase in gallbladder surgeries among users. That’s not a side effect. That’s a consequence. And the insurance denials? That’s not a barrier-it’s a feature. Keeps the masses out.
Imagine if we treated obesity like hypertension. You wouldn’t shame someone for taking blood pressure meds. You’d ask if they’re getting enough sleep, if they’re stressed, if they’ve got support. GLP-1 agonists aren’t the problem. The system that treats fatness like a moral failing is. These drugs are a band-aid on a broken system. But hey, sometimes a band-aid is all you’ve got.
My cousin went from 280 to 190 on Ozempic. Now she’s hiking, traveling, dating. But she’s also on a waiting list for a new prescription because her insurance dropped coverage. She’s not lazy. She’s just one bad policy away from losing it all. This isn’t a trend. It’s a lifeline for people who’ve been told their body is the problem.
Why do Americans always think a pill fixes everything? In Nigeria, we eat real food, walk everywhere, and sweat. No injections. No $1300/month. You don’t need magic. You need discipline. This is just capitalism selling hope to the desperate.
If you're taking this for weight loss, you're already failing. God gave us bodies to care for, not to chemically manipulate. Fasting, prayer, and discipline are the real path. This is not healing, it's rebellion against nature.