
This tool provides general risk assessment based on common thresholds. Always discuss your results with your healthcare provider who understands your full medical history.
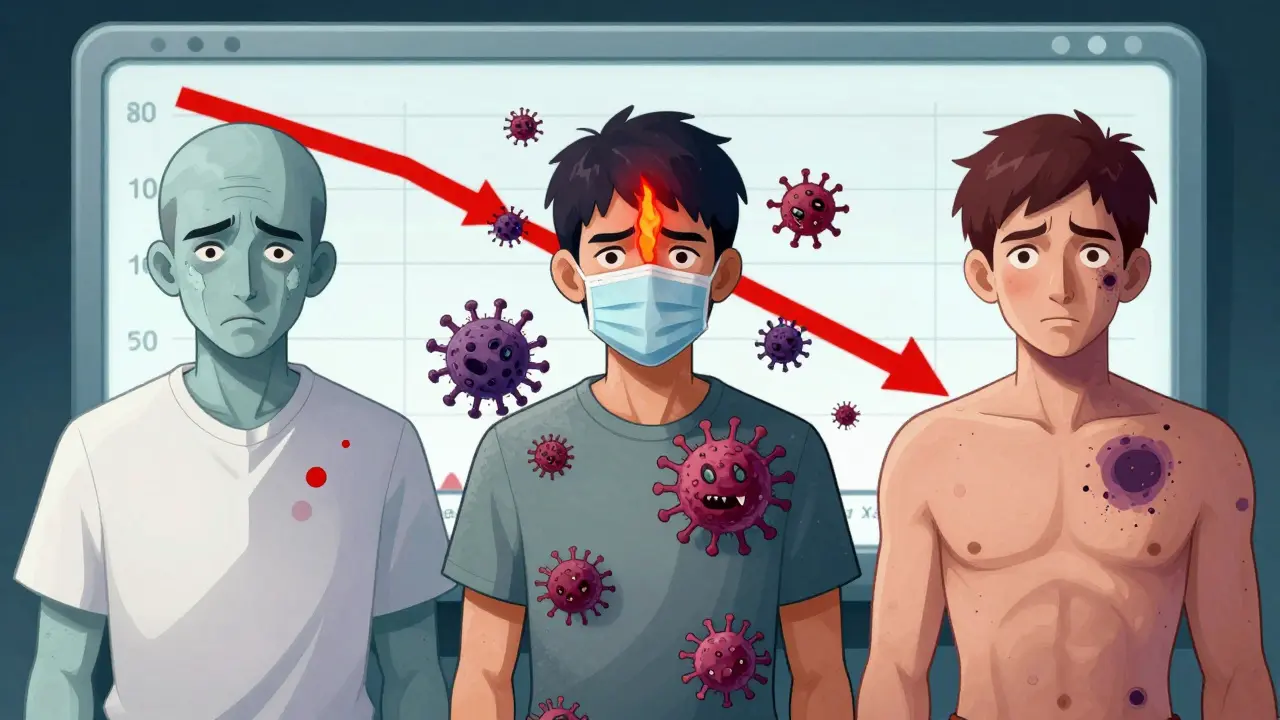
When a medication stops your bone marrow from making enough blood cells, it’s not just a lab result-it’s a real, life-changing risk. Bone marrow suppression isn’t rare. It’s one of the most common and dangerous side effects of treatments like chemotherapy, antibiotics, and immunosuppressants. For many people, it means canceled appointments, hospital visits, infections, and fear of bleeding out from a simple cut. This isn’t theoretical. It’s happening right now to thousands of patients every week.
These aren’t vague symptoms. They’re measurable, dangerous thresholds. The World Health Organization grades them from mild to life-threatening. And they’re not just numbers on a chart-they’re signals your body is in crisis.
The timing matters too. Most suppression hits 7-14 days after starting treatment. That’s when your blood counts hit their lowest point-the nadir. It’s not random. It’s the life cycle of your blood cells catching up to the drug’s damage.
Doctors check your blood with a complete blood count (CBC). Weekly tests during treatment are standard. Some hospitals, especially for kids, check every 48-72 hours. If your counts keep falling without explanation, they might do a bone marrow biopsy. But that’s rare. Most cases are caught early by routine blood work.
Key thresholds to watch:
And don’t ignore fever. A temperature over 38.3°C (101°F) during neutropenia is a medical emergency. It could mean sepsis. No waiting. No home remedies. Go to the ER.
Mild cases (Grade 1-2): Often just monitored. Your doctor might delay your next chemo dose or lower it. That’s not failure. It’s smart medicine.
Severe cases (Grade 3-4): You need action.
In extreme cases-when your marrow doesn’t recover-stem cell transplant may be the only option. Success rates? 65-75% with a matched sibling donor. It’s not a cure-all, but it’s hope.
Online forums like Reddit’s r/cancer and Smart Patients show the same pattern. Patients praise pegfilgrastim for keeping them out of the hospital. But they rage about the cost. One post reads: “I skipped my Neulasta shot because I couldn’t afford it. Got pneumonia two days later.”
And it’s not just chemo. One patient on Bactrim for a UTI ended up in the ICU with a platelet count of 8,000. “I didn’t know antibiotics could do this,” she said. “No one warned me.”

And if you’re on long-term immunosuppressants? Talk to your doctor about genetic testing. Some people carry mutations like TP53 that make them 3.7 times more likely to have severe suppression. Knowing that before treatment starts can change everything.
Future treatments are coming. Lixivaptan, approved in May 2023, cuts transfusion needs by 31%. Magrolimab is showing promise for anemia in bone marrow disorders. And researchers are building AI models that predict your risk before you even start treatment-using your genes, your age, your kidney function, your history.
This isn’t just about surviving treatment. It’s about staying on treatment. When patients get their counts back quickly, they finish their chemo. They live longer. They have better quality of life.
Bone marrow suppression isn’t a side effect you can ignore. It’s a signal. A warning. A call to act. The right questions, the right tests, the right support-you can turn a dangerous complication into a manageable part of your care.
In most cases, no. Bone marrow suppression caused by drugs is usually temporary. Once the medication is stopped or the dose is lowered, your marrow typically recovers within weeks. However, in rare cases-especially with long-term, high-dose chemo or certain genetic conditions-recovery can be incomplete. If counts don’t improve after stopping the drug, further testing is needed to rule out other causes like myelodysplastic syndrome or bone marrow failure.
No. Bone marrow suppression means your marrow is making too few blood cells, often due to a drug. Leukemia is cancer of the blood cells themselves-abnormal cells grow uncontrollably and crowd out healthy ones. While chemotherapy can sometimes lead to secondary leukemia years later, suppression itself is not cancer. It’s a side effect, not a diagnosis.
No. Iron, folic acid, or vitamin B12 won’t fix drug-induced bone marrow suppression. These supplements help only if your low counts are due to a nutritional deficiency. In most cases of medication-related suppression, your body has plenty of nutrients-it just can’t make blood cells. Taking extra supplements won’t help and could even interfere with your treatment. Always check with your oncologist before starting anything new.
At least once a week during active treatment with myelosuppressive drugs. For high-risk patients-like those on carboplatin or fludarabine-some clinics test every 3-4 days. Children and older adults often need more frequent monitoring. If your counts are stable and you’re on maintenance therapy, your doctor may space out tests. But never skip them without talking to your care team.
It’s a mix of genetics, age, kidney/liver function, and the specific drug and dose. Some people have gene variants that make them extra sensitive to certain drugs. For example, mutations in the TP53 gene increase risk by 3.7 times. Older adults, people with existing anemia, or those with poor nutrition are also more vulnerable. It’s not random-it’s predictable, and we’re getting better at identifying who’s at risk before treatment starts.
It depends. If your ANC is above 1,000 and you’re not bleeding, light activity is usually fine. But if your ANC is below 500, avoid crowds, public transit, and places with poor air quality. Wear a mask. Wash your hands constantly. Don’t go to restaurants with raw food. Your immune system is down. What’s a harmless trip to the grocery store for someone else could be life-threatening for you.
12 Responses
man i been on bactrim for a UTI last year and woke up one day with bruises all over my legs like i got jumped by a gang. doc said platelets at 12k. no one told me antibiotics could do this. i thought it was just for bacteria. turns out it's like a silent bomb in your marrow. scary as hell.
This is one of the clearest explanations I’ve ever read on bone marrow suppression. The breakdown of ANC thresholds, the timing of nadir, the distinction between nutritional deficiency and drug-induced suppression-everything is grounded in clinical reality. Thank you for not sugarcoating it. This should be required reading for anyone starting chemo or long-term immunosuppressants.
another overhyped medical article. everyone gets low counts. big deal. if you can’t handle a little anemia you shouldn’t be on chemo. stop being dramatic. the system is broken, not your blood.
I’ve seen this play out in oncology clinics. The real tragedy isn’t the suppression-it’s the silence around it. Patients aren’t warned. They’re handed a script and told to 'just stay strong.' But when your platelets hit 8k and you sneeze and bleed out of your nose? No one’s there. We need better pre-treatment counseling. Not just for cancer-anyone on azathioprine, trimethoprim, even some antivirals. This isn’t rare. It’s predictable. And we’re failing people by pretending it’s not.
It’s wild how much we rely on these drugs and how little we know about their hidden costs. I wonder if we’d still use them if we had to sign a waiver: 'This drug may turn your bone marrow into a ghost town.' The trade-off is survival vs. vulnerability. But who gets to decide that? And why is the burden always on the patient to ask the right questions? Shouldn’t the system be built to warn us before we even start?
they say suppression is temporary but what if its not what if the drugs are just masking a deeper truth your marrow was dying anyway and they just made you notice it maybe the real enemy isnt the chemo its the illusion that you were ever healthy to begin with
i just got my neulasta shot and honestly? it’s like magic. no more 3-day hospital stays. BUT $6500??? for a shot?? my insurance covers it but my friend skipped it to save $4k and got pneumonia. i cried. why does life-saving medicine cost more than a car?? 🤡
The real issue isn’t the drugs. It’s the fact that we treat patients like data points. You get a CBC, you get a number, you get a pill. No one sits down and says, 'Hey, your marrow might shut down in 10 days. Here’s what to watch for.' We’re not just under-informed-we’re systematically ignored. And the pharma companies? They’re fine with that. More injections. More transfusions. More revenue.
india has no access to neulasta or cosela. we get generic chemo and hope. my cousin got neutropenia and died in a village hospital because no one had a fever protocol. they said 'it was just infection' but it was his marrow giving up. this isn’t medicine. it’s lottery.
Just had my 3rd round of carboplatin. ANC hit 320. My nurse said 'avoid crowds' like it’s a suggestion. I didn’t go out for 14 days. Didn’t hug my dog. Didn’t go to the grocery. I even stopped answering the door. You don’t realize how much you take for granted until your immune system is on vacation.
I’m a nurse in oncology. I’ve seen patients recover from platelets at 4k. I’ve seen them bounce back after skipping Neulasta because they couldn’t afford it. I’ve seen families cry because they didn’t know a simple UTI antibiotic could do this. This post? It’s not just info-it’s a lifeline. Please share this with someone who’s about to start treatment. Knowledge is the only thing that can fight this silence.
I’m not mad. I’m just disappointed. I trusted my oncologist. I trusted the system. I didn’t know my own body could be turned against me by a pill. Now I keep a log. I track every CBC. I Google every drug. I don’t sleep unless I know my numbers. And I still wake up scared. This isn’t treatment. It’s a war inside your bones-and no one told me I’d have to fight it alone.