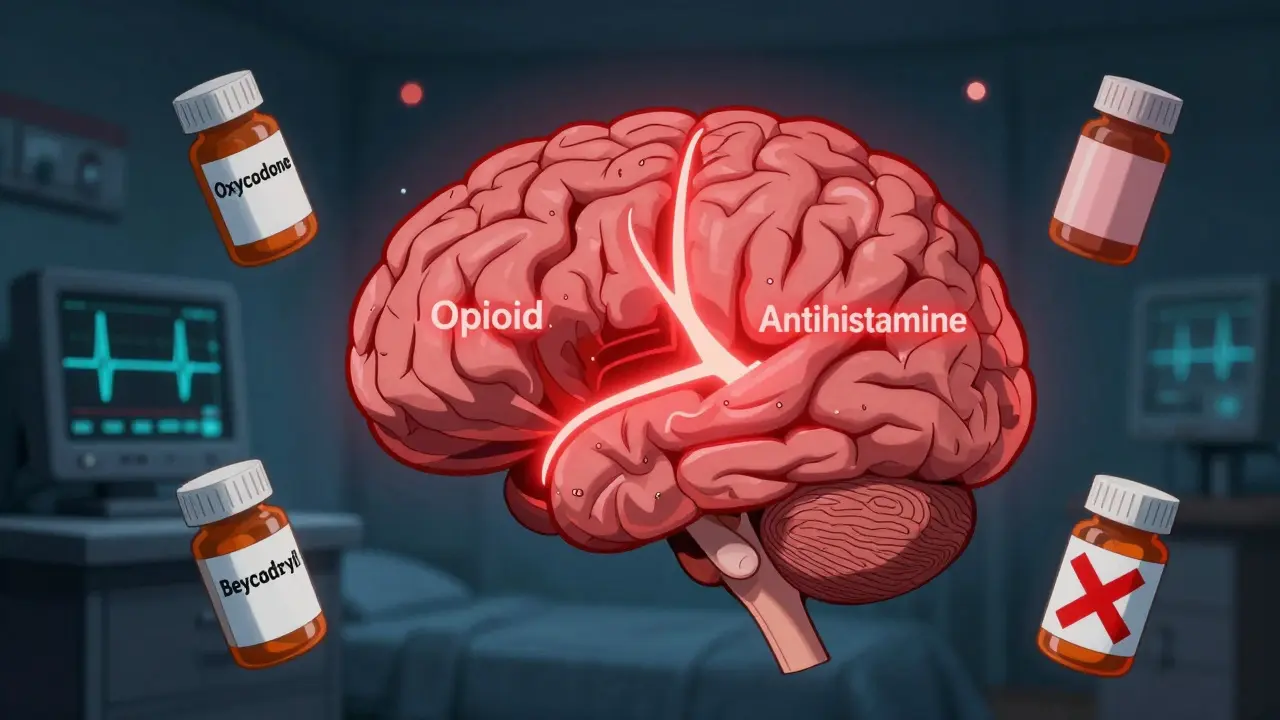
Check if your opioid pain medication can be safely combined with an antihistamine. This tool helps identify dangerous interactions and suggests safer alternatives.
Many people don’t realize that a common allergy pill can turn a prescribed painkiller into a life-threatening mix. Taking opioids like oxycodone or hydrocodone with over-the-counter antihistamines like diphenhydramine (Benadryl) or hydroxyzine (Atarax) doesn’t just make you sleepy-it can slow your breathing to a dangerous level, even stop it. This isn’t a rare accident. It’s a well-documented, preventable risk that kills people every year.
Studies show that when these drugs are taken together, the sedation isn’t just added-it’s multiplied. One study found that 20% to 60% of people on opioids alone report drowsiness. When you add a sedating antihistamine, that number jumps dramatically. The brain’s ability to trigger a breath when oxygen drops or CO2 rises becomes dangerously impaired. This isn’t theoretical. Emergency rooms see it regularly: patients found unresponsive after taking a painkiller and an allergy pill for itching or sleep.
First-generation antihistamines are the real problem. They have about 60-70% brain penetration. Second-generation antihistamines like fexofenadine (Allegra), loratadine (Claritin), or cetirizine (Zyrtec) have less than 1% brain penetration. That’s why Allegra is often recommended as a safe alternative-it treats allergies without the brain fog. But most people don’t know the difference. They just grab the cheapest bottle on the shelf, assuming “antihistamine” means the same thing everywhere.
People with COPD, sleep apnea, or heart disease are also at higher risk. Their bodies are already struggling to maintain oxygen levels. Adding a respiratory depressant pushes them past a tipping point. One study found that opioid-induced respiratory depression most often occurs in the first 24 hours after surgery-and patients with pre-existing lung or heart conditions were the most likely to suffer serious complications.
Even healthy young adults aren’t immune. A Reddit user shared a case of a 68-year-old man who became unresponsive after taking hydrocodone and Benadryl. He spent 36 hours in the ICU. Another patient on PatientsLikeMe fractured her hip after falling asleep while on oxycodone and Atarax. These aren’t outliers. They’re warning signs.

Unlike benzodiazepines, which can be reversed with flumazenil, there’s no direct antidote for antihistamine-induced CNS depression. Naloxone can reverse opioid effects-but it won’t fix the antihistamine part. That’s why some patients who get naloxone in the ER still need prolonged monitoring. In one physician survey, 32% of cases involving opioid-antihistamine interactions required naloxone, but many patients still needed hours of intensive care.
These aren’t “accidents.” They’re predictable outcomes of a system that treats OTC drugs as harmless. Pharmacists are required to hand out FDA-approved opioid medication guides-but only 34% of patients receive proper counseling about drug interactions, according to the CDC. That’s not enough.

If you’re a healthcare provider, screen every patient for OTC use. Use electronic health record alerts-hospitals that implemented them saw a 42% drop in adverse events. Follow CDC guidelines: avoid combining opioids with CNS depressants unless absolutely necessary, and if you must, use the lowest dose for the shortest time.
But the biggest gap remains patient education. The CDC and NIDA are funding new programs to teach people that “over-the-counter” doesn’t mean “safe with opioids.” Some clinics are starting to use pharmacogenetic testing to identify patients who metabolize opioids unusually slowly-making them more prone to overdose. Tests like Genelex’s Opioid Risk Panel cost around $349 and look at genes like CYP2D6 and CYP2C19 that affect how the body breaks down painkillers.
The bottom line: if you’re on an opioid, treat every sedating medication like a potential danger. Don’t assume your doctor knows you’re taking it. Don’t assume it’s harmless because it’s sold without a prescription. One pill can change everything.
No. Benadryl (diphenhydramine) is a first-generation antihistamine that significantly increases the risk of extreme drowsiness, slowed breathing, coma, or death when taken with opioids. Even if you’ve taken it before without issues, the risk builds up over time and can become deadly with a small dose increase. Always ask your doctor for a non-sedating alternative like Allegra or Claritin.
Benadryl (diphenhydramine) crosses into your brain and causes strong sedation, dizziness, and impaired breathing when combined with opioids. Allegra (fexofenadine) barely enters the brain-it’s designed to treat allergies without drowsiness. At standard doses, Allegra has negligible sedative effects and is considered safe to use with opioids under medical supervision.
Many doctors assume patients know OTC meds are risky, or they don’t ask about them. A CDC study found only 34% of opioid patients receive full counseling on drug interactions. Patients often don’t mention taking antihistamines because they don’t think of them as “medications.” Always volunteer that information-don’t wait to be asked.
Yes. Zyrtec (cetirizine) and Claritin (loratadine) are second-generation antihistamines with very low brain penetration. They cause little to no sedation at standard doses and are generally safe to use with opioids. Still, always check with your doctor or pharmacist, especially if you’re elderly or have breathing problems.
Call emergency services immediately. If naloxone is available, administer it-though it only reverses the opioid part, not the antihistamine. Stay with the person, keep them on their side, and monitor their breathing until help arrives. Do not try to wake them by shaking or slapping. This is a medical emergency.
14 Responses
Just had to share this-my grandma took Benadryl with her oxycodone for years and never said a word. She’s fine now, but I freaked out when I found out. 🤯 Thanks for spelling this out so clearly. I printed this and taped it to her pill organizer. 🙏
Oh wow, another ‘don’t mix drugs’ PSA. How original. People die from eating too many apples too, but nobody’s banning fruit. You’re just fearmongering to feel superior. 🤡
One must interrogate the epistemological foundations of pharmaceutical safety narratives. The very notion of ‘OTC = harmless’ is a neoliberal construct designed to externalize risk onto the individual consumer. The real tragedy isn’t the drug interaction-it’s the commodification of bodily autonomy under the guise of informed consent. 🤔
Look, I get it, people are dumb, but let’s not pretend this is some new revelation. I’ve been a pharmacist for 22 years and I’ve seen this exact scenario play out in every town from Manchester to Bristol. It’s not the drugs, it’s the culture of ignoring labels. People treat medicine like candy-pop a pill, feel better, move on. And then when it goes wrong, they blame the doctor, the pharmacy, the government. But nobody takes responsibility for reading the damn bottle. I’ve had patients cry because their ‘natural sleep aid’ killed their husband, and I just sat there thinking: you knew what was in it. You just didn’t care enough to ask. This isn’t a medical crisis. It’s a moral one.
soooo benadryl is bad now but adderall is fine with opioids right? 😏
Everyone’s acting like this is news. I’ve been telling people this since 2018. You think your ‘sleep aid’ is harmless? Try telling that to the guy in the morgue whose autopsy says ‘opioid + diphenhydramine’. And now you want a medal for pointing it out? Grow up.
Thank you so much for writing this. I had no idea. I’ve been taking Zyrtec with my tramadol for months and thought I was being smart. I just switched to Allegra today. 💙 I’m sharing this with my entire family. You saved someone’s life today.
The pharmacokinetic synergy between mu-opioid receptor agonism and H1 antagonism induces synergistic CNS depression via GABAergic modulation and respiratory center suppression. The clinical implications are non-trivial, particularly in polymorphic CYP2D6 metabolizers. This isn’t ‘dangerous’-it’s biologically deterministic. The failure lies in the lack of pharmacogenomic screening in primary care. End of discussion.
hey i just want to say thank you for this. i took benadryl with my pain meds last week and felt super weird but i thought it was just the painkillers. i stopped it right away. you’re a lifesaver. sorry for the typos, typing on my phone 😅
In the grand tapestry of human suffering, we often mistake the symptom for the disease. The real issue is not the combination of drugs, but the alienation that drives people to self-medicate. We live in a world where pain is met with pills, not presence. Perhaps the antidote is not a safer antihistamine, but a society that listens.
Thank you for your dedication to public safety. This information must be disseminated through all healthcare channels. I have already emailed my local clinic to request inclusion in their patient education packets. Your work is appreciated.
Man, I’ve been telling my cousin for years not to mix Benadryl with his codeine. He thought I was being dramatic. Now he’s on a breathing machine. I’m glad someone’s finally putting this out there. 🙏
lol so what? people die from water too.
As an American citizen, I find it unacceptable that our healthcare system allows such preventable tragedies to occur. This is a failure of institutional responsibility. Every pharmacy in this country should be required to display warning signs next to all first-generation antihistamines. This is not a suggestion. This is a national imperative.