Psychiatric Medications: Class Interactions and Dangerous Combinations
When you’re taking more than one psychiatric medication, it’s not just about how each drug works alone-it’s about what happens when they meet. Some combinations can make you feel better. Others can land you in the hospital. The difference often comes down to a few hidden interactions that many patients-and even some providers-don’t see coming.
Why Psychiatric Drug Interactions Matter More Than You Think
Psychiatric medications don’t float around in your body in isolation. They talk to each other. And sometimes, they argue. The most common battleground? Neurotransmitters-chemical messengers like serotonin, norepinephrine, and dopamine. When two drugs both crank up serotonin, for example, your brain can get overloaded. That’s not just a side effect. It’s serotonin syndrome, a condition that can kill.
According to the American Association of Psychiatric Pharmacists, 30% to 50% of adverse drug events in psychiatric care come from these kinds of interactions. That’s not rare. That’s routine. And most of them happen within the first week of adding a new medication. The first dose is the most dangerous one.
High-Risk Classes and the Medications That Cause Trouble
Not all psychiatric drugs are created equal when it comes to interactions. Some are quiet. Others are loud. Here’s who to watch:
- MAO inhibitors (MAOIs) like phenelzine and tranylcypromine: These are the most dangerous. They stop your body from breaking down serotonin. Combine them with SSRIs, SNRIs, or even some OTC cold meds, and you’re playing Russian roulette with your nervous system.
- SSRIs like fluoxetine, sertraline, and fluvoxamine: Fluvoxamine is especially risky. It blocks key liver enzymes (CYP1A2, 2C19, 3A4), meaning it can make other drugs build up to toxic levels. Even if you’re on a low dose of something else, fluvoxamine can turn it into an overdose.
- SNRIs like venlafaxine and duloxetine: Less risky than MAOIs, but still dangerous with other serotonergic drugs. Venlafaxine can raise blood pressure, and combining it with stimulants or decongestants can spike it dangerously high.
- TCAs like amitriptyline and nortriptyline: These old-school antidepressants dry you out-literally. They block acetylcholine, which can cause confusion, constipation, and urinary retention. Mix them with antihistamines, antipsychotics, or even some heart meds, and you’re asking for trouble.
- Lithium: It’s a mood stabilizer, but its window between helpful and toxic is razor-thin. Normal levels? 0.6-1.0 mmol/L. Above 1.2? Emergency. NSAIDs like ibuprofen can push lithium levels up by 25-50%. Even a few days of extra Advil can turn a stable patient into a medical crisis.
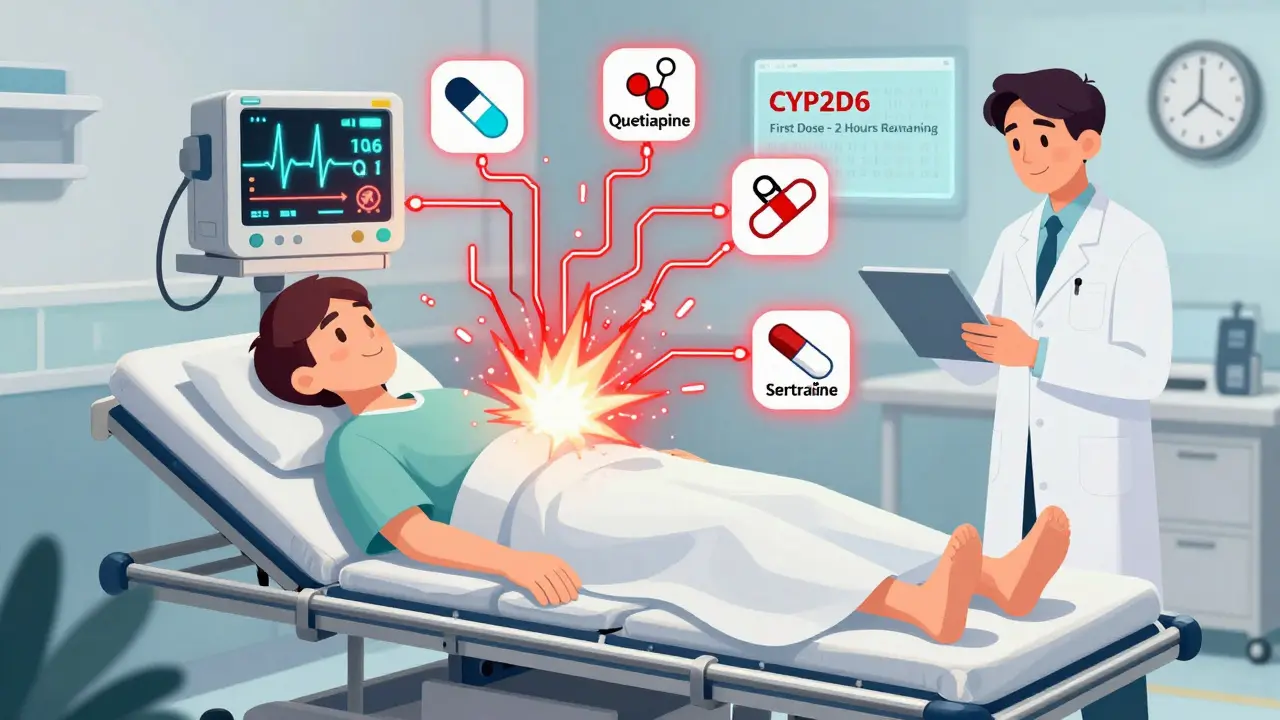
- Atypical antipsychotics like quetiapine and risperidone: Quetiapine is relatively safe. But others? They can cause QT prolongation, which means your heart rhythm goes off. Combine them with certain antibiotics, antifungals, or even some antidepressants, and you risk sudden cardiac arrest.
The Deadliest Combo: Serotonin Syndrome
Serotonin syndrome isn’t a myth. It’s real. And it kills. The classic sign? A triad:
mental changes (agitation, confusion),
autonomic overdrive (sweating, fever, rapid heartbeat), and
neuromuscular issues (tremors, muscle rigidity, overactive reflexes).
The worst offenders? Any combo of an MAOI with an SSRI or SNRI. That’s a recipe for disaster. But it’s not just prescription drugs. Even over-the-counter supplements like St. John’s wort, tryptophan, or dextromethorphan (found in cough syrups) can trigger it when mixed with antidepressants.
Studies show mortality rates between 2% and 12% in severe cases. And it often happens fast-within hours of taking a new pill. That’s why first-dose monitoring is non-negotiable. If you’re starting a new combo, you need to be watched for at least 2-4 hours after the first dose. No exceptions.

Other Dangerous Combinations You Might Not Know About
- Lithium + NSAIDs: As mentioned, ibuprofen, naproxen, or even aspirin can push lithium into toxic range. If you’re on lithium and get a headache, skip the Advil. Use acetaminophen instead.
- SSRIs + Warfarin: Fluoxetine and fluvoxamine can boost warfarin levels by 20-30%, increasing bleeding risk. If you’re on blood thinners, your INR needs weekly checks for the first month after starting an SSRI.
- TCAs + Alcohol: This combo doesn’t just make you sleepy. It can cause severe sedation, loss of coordination, and even respiratory depression. It’s like taking a sedative and a depressant at the same time.
- Clozapine + CYP1A2 inhibitors: Clozapine is a powerful antipsychotic for treatment-resistant schizophrenia. But it’s broken down by CYP1A2. Smoking helps clear it. Quitting smoking? Levels can spike overnight. Same thing if you start fluvoxamine or ciprofloxacin. You need frequent blood level checks.
- Carbamazepine + SSRIs: Carbamazepine lowers the levels of many antidepressants. Add an SSRI and you might think it’s not working-when really, your body is flushing it out too fast.
How to Stay Safe: Practical Rules for Patients and Providers
There’s no magic bullet, but there are clear steps that save lives:
- Know your meds. Don’t just take what’s prescribed. Ask: What does this do? What does it interact with? Write it down.
- Use low-interaction drugs when possible. Sertraline and citalopram are safer SSRIs than fluvoxamine. Quetiapine is safer than olanzapine. Vilazodone has fewer interactions than most. Ask your doctor if a lower-risk option exists.
- Check every new medication. Even a Z-pack antibiotic or a new painkiller can mess with your psychiatric meds. Use a reliable drug interaction checker-like Micromedex or Lexicomp-before you take anything new.
- Monitor your labs. Lithium? Check levels every 3 months, or after any dose change. Clozapine? Weekly blood counts for the first 6 months. Valproate? Liver tests every 3 months. Don’t skip these.
- Track symptoms. Use simple tools: PHQ-9 for depression, GAD-7 for anxiety, AIMS for movement side effects. If your score jumps, something’s off.
- Never stop or start meds on your own. Even a small change can trigger an interaction. Tell your prescriber before you take anything new.
What’s New in 2026? Technology Is Helping
In 2024, the National Institute of Mental Health began testing AI models that predict individual interaction risks based on your genetics, meds, and medical history. Early results show they can flag 80% of high-risk combos before they happen.
Digital tools are already in use. Some clinics use real-time alerts in their EHRs that pop up when a new prescription might clash with existing ones. One study showed a 37% drop in serious interactions when these systems were used with proper clinician training.
Genetic testing is also becoming more common. If you have a slow CYP2D6 or CYP2C19 enzyme, certain antidepressants won’t work-or could poison you. Testing for these variants is now recommended by the Clinical Pharmacogenetics Implementation Consortium (CPIC) before starting SSRIs or TCAs.
Bottom Line: Don’t Guess. Check.
Psychiatric medications save lives. But they can also end them-if you don’t know what you’re mixing. The truth is, no one expects a simple antidepressant to cause a heart rhythm problem or a fever that spikes to 105°F. But it happens. Every day.
The solution isn’t avoiding meds. It’s being smart about them. Know your drugs. Know your risks. Ask questions. Keep a list. Track your symptoms. And never assume a new pill is harmless just because it’s prescribed.
Your brain is complex. Your meds are powerful. Treat their interactions with the seriousness they deserve.
Can I take over-the-counter cold medicine with my antidepressant?
Be very careful. Many OTC cold and flu meds contain dextromethorphan or pseudoephedrine. Dextromethorphan can trigger serotonin syndrome when taken with SSRIs, SNRIs, or MAOIs. Pseudoephedrine can raise blood pressure dangerously when combined with MAOIs or TCAs. Always check with your pharmacist or doctor before taking any OTC product.
Is it safe to drink alcohol while on psychiatric meds?
It’s rarely safe. Alcohol can amplify sedation from TCAs, antipsychotics, and benzodiazepines. It can worsen depression and anxiety over time. With MAOIs, alcohol can cause dangerous spikes in blood pressure. Even moderate drinking increases the risk of falls, confusion, and liver damage. If you’re on psychiatric meds, it’s best to avoid alcohol entirely.
Why do some antidepressants cause weight gain and others don’t?
It depends on how they affect brain receptors. Medications like mirtazapine and paroxetine block histamine and serotonin receptors in ways that increase appetite. Others, like bupropion and vilazodone, have little effect on these receptors and are less likely to cause weight gain. If weight gain is a concern, ask your doctor about alternatives with lower metabolic impact.
How long should I wait between stopping an MAOI and starting an SSRI?
You need at least 14 days after stopping an MAOI before starting an SSRI. For fluoxetine, which stays in your system longer, wait 5 weeks. This washout period is critical to prevent serotonin syndrome. Never rush this step-even if you feel worse during the gap.
Can genetic testing help me avoid bad drug interactions?
Yes. Testing for CYP2D6 and CYP2C19 enzyme activity can show if you’re a slow, normal, or fast metabolizer of certain antidepressants. Slow metabolizers risk toxicity from standard doses. Fast metabolizers may get no benefit. This testing is now recommended before starting SSRIs, TCAs, or antipsychotics like risperidone. It’s not perfect-but it reduces trial-and-error.
What should I do if I think I’m having serotonin syndrome?
Call 911 or go to the ER immediately. Symptoms include high fever, rapid heartbeat, muscle stiffness, confusion, or seizures. Don’t wait. Serotonin syndrome can progress rapidly. Tell the medical team exactly what medications and supplements you’re taking. Early treatment with serotonin blockers like cyproheptadine can be life-saving.
Are herbal supplements safe to take with psychiatric meds?
No, not without checking. St. John’s wort can cause serotonin syndrome with SSRIs. Kava can increase sedation with benzodiazepines. Valerian can amplify the effects of antipsychotics. Even omega-3s can thin the blood and interact with lithium. Always disclose every supplement to your prescriber-even if you think it’s "natural" or "harmless."
Next Steps: What to Do Today
- Make a complete list of every medication and supplement you take-including doses and why you take them.
- Bring it to your next appointment and ask: "Are any of these combinations dangerous?"
- If you’re on lithium, MAOIs, clozapine, or warfarin, ask if your labs are up to date.
- Download a free drug interaction checker app (like Medscape or Epocrates) and use it before taking anything new.
- Set a reminder to review your meds every 3 months. Your body changes. Your risks change too.
Psychiatric medications aren’t magic. They’re tools. And like any tool, they’re safest when you understand how they work-and what happens when they meet other tools. Stay informed. Stay vigilant. Your brain deserves nothing less.

10 Responses
This post is terrifying and amazing at the same time.
Like, I didn’t realize my ibuprofen could turn my lithium into a time bomb.
Now I’m checking every pill I’ve ever taken.
Thanks for the wake-up call.
I’m so glad someone finally laid this out plainly.
I’ve been on sertraline and occasional cold meds for years and never thought twice.
Now I’m scared to even take NyQuil.
Thank you for making me safer.
Yo, this is the kind of shit they don’t teach you in med school unless you’re in psychopharm hell.
MAOIs + SSRIs = instant serotonin tsunami.
And don’t even get me started on fluvoxamine-it’s the silent killer of CYP enzymes.
My cousin ended up in ICU after mixing St. John’s wort with his escitalopram.
He thought it was ‘natural’ so it was ‘safe.’
Bro, natural doesn’t mean non-toxic.
My grandma’s chamomile tea could kill you if you’re on MAOIs.
Also, clozapine + quitting smoking? That’s not a lifestyle change, that’s a cardiac roulette spin.
And why do we still let people self-medicate with OTC crap like dextromethorphan?
It’s like handing a loaded gun to someone with a history of depression.
PS: If you’re on lithium, acetaminophen is your BFF. Advil? Your worst enemy.
PPS: Genetic testing isn’t sci-fi anymore. Get your CYP2D6 checked before you take another pill.
PPPS: This post should be mandatory reading for every psych patient. Seriously.
So let me get this straight.
We give people brain-altering chemicals, then tell them not to take cold medicine.
And if they do? They die.
Meanwhile, the FDA approves new antidepressants every year but won’t ban cough syrup with dextromethorphan.
Classic.
Also, ‘natural’ supplements are just pharmaceuticals with better PR.
St. John’s wort? It’s Prozac with a yoga mat.
Thanks for the honesty, though.
At least someone’s not sugarcoating it.
I’ve been on lithium for 12 years.
I never knew ibuprofen could push me into toxicity.
I’ve been taking it for migraines since college.
Now I’m switching to Tylenol.
And I’m printing this out to give to my doctor.
Thank you for writing this.
It’s the kind of info that saves lives.
And it’s not even that complicated.
Just… nobody tells you.
Maybe because they assume you’ll figure it out.
But you won’t.
Not unless someone holds your hand and says: ‘Hey, this thing you think is harmless? It’s not.’
So thank you.
Really.
My cousin died from serotonin syndrome.
He was on Lexapro.
He took a cough syrup.
He was 23.
Don’t take risks.
Ever.
Per CPIC guidelines, CYP2C19 poor metabolizers are at elevated risk for SSRI toxicity, particularly with fluvoxamine and citalopram, due to reduced hepatic clearance.
Pharmacogenomic screening is now Class I recommendation for first-line antidepressant selection.
Yet <15% of clinics implement it routinely.
Systemic inertia remains the greatest barrier to precision psychiatry.
Also, MAOI washout periods are non-negotiable.
Fluoxetine’s half-life is 7 days. Don’t be that guy.
I’m a psychiatrist and I’ve seen this too many times.
Patients come in with tremors, sweating, and confusion.
We ask about new meds.
They say, ‘Oh, I just started this herbal thing.’
It’s always St. John’s wort.
Or dextromethorphan.
Or ibuprofen.
Or they stopped their antipsychotic cold turkey and started an SSRI.
It’s not the meds that are dangerous.
It’s the silence around them.
Doctors don’t have time.
Patients don’t know to ask.
And pharmacies? They print a 3-page warning sheet that no one reads.
This post? It’s the kind of thing that should be on every pharmacy counter.
Not just in a blog.
And yes - genetic testing helps.
My clinic started doing CYP2D6 tests 2 years ago.
Our adverse event rate dropped by 40%.
It’s not magic.
It’s science.
And we’re still not using it enough.
Psych meds aren’t candy.
They’re not ‘just pills.’
They’re molecular grenades with safety pins pulled.
One wrong move - and your brain goes nuclear.
And yet we treat them like aspirin.
‘Oh, I’ll just take this cold medicine.’
‘I’ll skip my mood stabilizer for a few days.’
‘I’ll try this new supplement - it’s all natural!’
NO.
NO.
NO.
You are not a lab rat.
Your brain is not a test tube.
Every interaction matters.
Every dose.
Every day.
So write it down.
Ask the questions.
Check the apps.
And if you’re on lithium? Don’t even think about ibuprofen.
Use Tylenol.
And if you’re on MAOIs? Don’t even look at a banana.
Just… please.
Stay alive.
You’re worth it.
Bro, this is peak neuropharm chaos 😵💫
MAOIs + SSRIs = serotonin apocalypse 🌪️
Fluvoxamine = enzyme assassin 🗡️
Lithium + Advil = ER party 🚑
And don’t even get me started on clozapine + quitting smoking 😳
Genetic testing? Yes please 🧬
But why is this not standard??
Why are we still playing Russian roulette with brain chemistry??
We have AI that can predict this now.
So why aren’t we using it??
Someone’s making money off trial and error.
And we’re the lab rats.
Wake up.
Check your meds.
Don’t be a statistic.
❤️🩹