After a colonoscopy finds and removes polyps, many people wonder: when do I need another one? It’s not a one-size-fits-all answer. The timing depends on what kind of polyps were found, how many, how big they were, and even how well the bowel was cleaned before the procedure. Getting the next colonoscopy too soon wastes time, money, and causes unnecessary stress. Waiting too long could miss something dangerous. The good news? Most people don’t need another colonoscopy for years - if at all.
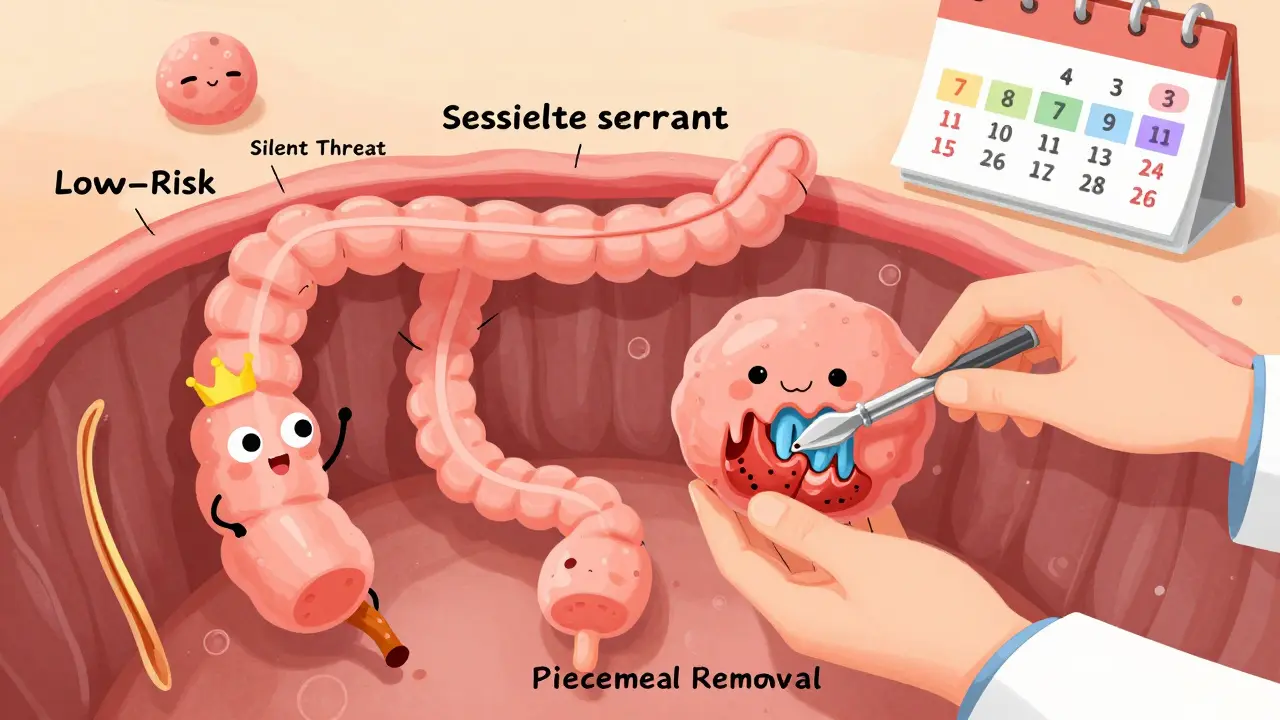
Polyps aren’t all created equal. Some are harmless, others are warning signs. The two main types you’ll hear about are adenomas and serrated polyps. Adenomas are the most common precancerous growths. If left alone, they can slowly turn into colorectal cancer over 10-15 years. Serrated polyps - especially sessile serrated lesions (SSLs) - are trickier. They grow differently, often hiding in the right side of the colon, and can become cancerous faster than adenomas. Then there are hyperplastic polyps, which are almost always benign unless they’re large or in certain locations.
Doctors look at three things to decide your next steps: type, size, and number. A 5-mm adenoma is very different from a 15-mm one. One small polyp is not the same as five. And a polyp removed in one piece is safer than one cut into pieces during removal.
If you had 1 or 2 small adenomas (each less than 10 mm), your risk of developing colon cancer in the next decade is nearly the same as someone with a completely normal colonoscopy. That’s why the latest guidelines from the U.S. Multi-Society Task Force (2020) recommend waiting 7 to 10 years for your next colonoscopy. This was a big change from the old 5-year rule.
Many doctors still recommend 5 years out of habit - or fear of missing something. But data shows that 98.7% of people with 1-2 small adenomas remain cancer-free at 10 years. That’s almost identical to the 99.3% rate for people with no polyps at all. Extending the interval reduces unnecessary procedures and cuts down on risks like bowel perforation or complications from sedation.
If you had 3 or 4 adenomas, all under 10 mm, the risk goes up. You’re not in the high-risk group, but you’re not low-risk either. The current recommendation is a follow-up in 3 to 5 years. The exact timing depends on other factors - like whether your bowel prep was good or if the polyps were hard to see.
Now, if you had 5 or more adenomas, no matter their size, you’re in a higher-risk category. That means your next colonoscopy should be in 3 years. Same goes if you had any adenoma that was 10 mm or larger. Size matters. A 12-mm polyp carries more risk than a 7-mm one, even if they look similar under the scope.
Sessile serrated lesions (SSLs) are becoming more common and are now a major focus in colon cancer prevention. If you had 1 or 2 SSLs smaller than 10 mm, you should get another colonoscopy in 5 to 10 years. That’s the same as low-risk adenomas. But if you had 3 to 4 SSLs, you need to come back in 3 to 5 years. Five or more? Back in 3 years.
Here’s the catch: SSLs are easy to miss. They’re flat, pale, and blend into the colon lining. If the bowel prep was poor, or if the doctor didn’t take enough time examining the right side of the colon, your risk of a missed lesion goes up. That’s why some doctors will shorten the interval if they’re unsure about the quality of the exam.

When a polyp is bigger than 20 mm, it’s often removed in pieces - called piecemeal resection. This increases the chance that some tissue is left behind. That’s why follow-up is urgent. The U.S. guidelines say: come back in 6 months. The European guidelines give a window of 3 to 6 months. Either way, this isn’t a suggestion - it’s a requirement.
Why 6 months? That’s the window where you can catch any leftover tissue before it turns into something worse. Waiting longer than that could mean missing early signs of recurrence. This is especially important if the polyp had high-grade dysplasia or villous features.
Most hyperplastic polyps (HPs) are harmless. But if one is 10 mm or larger, or if it’s in the right side of the colon, it could be mistaken for an SSL. In those cases, experts recommend a follow-up in 3 to 5 years. If the doctor isn’t sure whether it’s an HP or an SSL - or if the removal wasn’t complete - they’ll lean toward the 3-year mark.
Don’t assume a small HP means you’re in the clear. If you have multiple HPs, especially in the ascending colon, your doctor might treat them like serrated lesions. Always ask: “Was this a true hyperplastic polyp, or could it be something more?”
This rare condition means you have a lot of serrated polyps scattered throughout your colon - sometimes dozens. It runs in families and dramatically increases cancer risk. If you’ve been diagnosed, you need annual colonoscopies until age 75. Some guidelines allow stretching to every 2 years if no large polyps are found, but most experts stick with yearly checks. This isn’t optional. It’s life-saving.
Even though guidelines have been clear since 2020, a 2020 study at a Veterans Affairs hospital found only 18.6% of gastroenterologists followed the extended 7-10 year interval for low-risk polyps. Most still said “5 years.” Why? Fear. Legal concerns. Lack of training. Or just old habits.
Another problem: primary care doctors often manage follow-up care, but many don’t know the latest rules. A 2022 survey found only 37% of gastroenterologists could correctly identify all the risk categories. For serrated polyps? Only 28.5% got it right.
Patients are left confused. One person gets told to come back in 5 years. Another, with the same polyps, is told 10 years. The inconsistency leads to over-testing - and unnecessary stress.
There are now apps and EHR tools built to help. Polyp.app, developed by Massachusetts General Hospital, lets doctors input polyp details and instantly get the correct interval. Epic and Cerner systems now include automated reminders based on your procedure report. But these tools only work if the data is entered correctly.
Ask for a copy of your colonoscopy report. Look for these key terms: “adenoma,” “sessile serrated lesion,” “size,” “number,” “resection method.” If it’s not clear, call your doctor’s office. Don’t assume they’ll remember the details.
Some people avoid colonoscopies because they’re expensive, inconvenient, or scary. If you’re due for a follow-up but hesitant, talk to your doctor about alternatives. Stool-based tests like FIT or Cologuard can be used in some cases - but they’re not replacements for surveillance after polyps. If you’ve had polyps, colonoscopy is still the gold standard. It lets your doctor see and remove anything suspicious in real time.
Skipping your follow-up because you’re nervous isn’t worth the risk. Colon cancer is preventable - if caught early. And surveillance colonoscopies are the most effective way to stop it before it starts.
Right now, we count polyps and measure size. In the future, we might use blood or stool tests to check for DNA changes that signal higher cancer risk. Clinical trials are already testing molecular markers - like methylation patterns - to predict who needs a colonoscopy in 3 years versus 10. This could mean fewer tests for low-risk people and more targeted checks for those who really need them.
For now, stick to the guidelines. They’re based on millions of data points and decades of research. Don’t let outdated advice or confusion lead you to wait too long - or come back too soon.
If you had one or two small adenomas (less than 10 mm), you should schedule your next colonoscopy in 7 to 10 years. This is based on the 2020 U.S. guidelines, which found that cancer risk for these patients is nearly the same as for people with no polyps. Many doctors still say 5 years, but the extended interval is now the standard for low-risk cases.
Yes, but only if they’re large or numerous. One or two small sessile serrated lesions (SSLs) under 10 mm follow the same 5-10 year rule as low-risk adenomas. But if you have three or more SSLs, or any SSL that’s 10 mm or larger, your next colonoscopy should be in 3 to 5 years. Five or more SSLs mean you need another one in 3 years. SSLs are harder to detect and can turn cancerous faster, so they’re treated more carefully.
If a polyp larger than 20 mm was removed in pieces (piecemeal resection), you need a follow-up colonoscopy in 6 months. This is because leftover tissue can regrow or develop into cancer. Waiting longer increases risk. Some European guidelines say 3-6 months, but 6 months is the standard in the U.S., Japan, and Korea. Don’t delay this one.
No - not after polyps have been found. Stool tests like FIT or Cologuard are great for initial screening in people with no history of polyps. But once you’ve had polyps removed, colonoscopy is the only reliable way to check for new growths. Stool tests can’t see or remove polyps. They also miss flat or small lesions. Your doctor will still require a colonoscopy for surveillance.
Guidelines changed in 2020, but not everyone updated their practice. Many doctors still follow the old 5-year rule out of habit, fear of lawsuits, or lack of training. Some are unsure how to classify serrated polyps. Also, if your bowel prep was poor or the exam was incomplete, your doctor may recommend an earlier follow-up - even if your polyps were low-risk. Always ask why they’re recommending a specific interval.
Family history changes everything. If you have a first-degree relative (parent, sibling, child) with colon cancer or advanced polyps before age 60, you’re considered higher risk - even if your polyps were small. In that case, your doctor will likely recommend a 5-year interval regardless of polyp type. Always share your family history with your gastroenterologist before your colonoscopy.
Yes. If you notice blood in your stool, unexplained weight loss, persistent abdominal pain, or a change in bowel habits (like new constipation or diarrhea lasting more than a few weeks), don’t wait for your scheduled colonoscopy. Call your doctor. These could be signs of a new problem. Surveillance intervals are for prevention - not emergency diagnosis.
12 Responses
Why do doctors still say 5 years? It’s 2024. The guidelines changed four years ago. If you’re not keeping up, stop giving medical advice. I had two small adenomas and my doc said 10 years. I told him to read the 2020 U.S. guidelines. He did. Now he sends patients there. Stop being lazy.
This is such a clear, well-structured breakdown. I’ve been terrified of colonoscopies for years, but after reading this, I actually feel empowered. Knowing the science behind the timelines takes away the guesswork. Thank you for sharing this - I’m printing it out and bringing it to my next appointment.
Oh my gosh, I just realized I missed my follow-up by two years because my PCP said ‘5 years’ and I trusted them. I didn’t even know there was a difference between adenomas and serrated polyps. I’m calling my GI right now. I’m so mad at myself for waiting. But also… thank you. This post literally could’ve saved me from cancer.
The tension between guideline adherence and clinical habit is fascinating. It speaks to a deeper issue: medicine often prioritizes certainty over evidence. The 7–10 year window isn’t just statistical-it’s philosophical. It assumes that human bodies, like ecosystems, heal and stabilize over time. Yet fear overrides patience. We treat prevention like an emergency.
bro i just got my report and it said '3 hyperplastic polyps' and my doc said 'come back in 3 years' but i read this and now i'm confused are they bad or nah??
Let me cut through the noise: if you had one small adenoma, you’re fine for 7–10 years. Period. The 5-year myth is killing healthcare budgets and scaring people for no reason. I’ve seen patients get colonoscopies every 3 years because their doctor was scared of a lawsuit. That’s not medicine. That’s fear-based billing. Stop overtesting. Trust the data. Your colon will thank you.
Wow. So now the rule is: if you’re a doctor who doesn’t want to think, just say ‘5 years.’ If you’re a patient who doesn’t want to think, just believe them. Meanwhile, the science quietly moves forward. Classic. I’m just glad I read this instead of trusting my GI’s 2015 notes.
What if you’re one of those people who got a polyp removed and then spent the next 8 years avoiding mirrors because you’re scared of your own colon? 😅 I mean… yeah, 7–10 years is fine, but what if you just want to feel safe? Is it wrong to get one every 5 years just to calm your nerves? 🤔
my doc said 5 yrs but i read this and now i think 7 is fine. should i push back?
While I appreciate the clinical precision of this post, I must emphasize that the psychological burden of surveillance colonoscopy should not be underestimated. The institutional inertia toward outdated protocols may, in fact, exacerbate patient anxiety rather than alleviate it. One must consider not only the physiological but the phenomenological dimension of medical care.
So basically, if you’re rich and have a good doctor, you wait 10 years. If you’re poor and your doctor is lazy, you get scammed into a 5-year one. Great. Just great. 😒
It’s ironic that we’ve reduced a complex biological process - the transformation of mucosal epithelium into invasive carcinoma - to a spreadsheet of polyp counts and millimeter measurements. The human colon is not a math problem. It’s an ecosystem shaped by microbiota, diet, epigenetics, and stress. To reduce it to ‘one adenoma = 7 years’ is not just reductive - it’s dangerously simplistic. And yet, here we are, treating colon cancer prevention like a spreadsheet optimization problem. We’ve lost the forest for the trees. And the trees? They’re still growing.