
When a lump shows up in your neck, or your doctor feels something unusual during a checkup, the first thing they’ll likely recommend is a thyroid ultrasound. It’s not a scary procedure-it’s quick, painless, and doesn’t use radiation. But what happens during that scan? And why does it matter so much for figuring out if a nodule might be cancer?
Thyroid ultrasound uses high-pitched sound waves, not X-rays, to build a real-time picture of your thyroid gland. It’s like taking a video of the inside of your neck, but with sound. The machine sends out waves through a handheld device (called a transducer) pressed gently against your skin. These waves bounce off tissues and return as echoes, which the computer turns into a detailed image.
This isn’t just about finding lumps. It’s about seeing the details: whether a nodule is solid or filled with fluid, how dark or light it looks compared to surrounding tissue, its shape, edges, and whether it has tiny white spots called microcalcifications. These features aren’t random-they’re clues. And doctors have spent decades studying them to figure out which ones raise red flags.
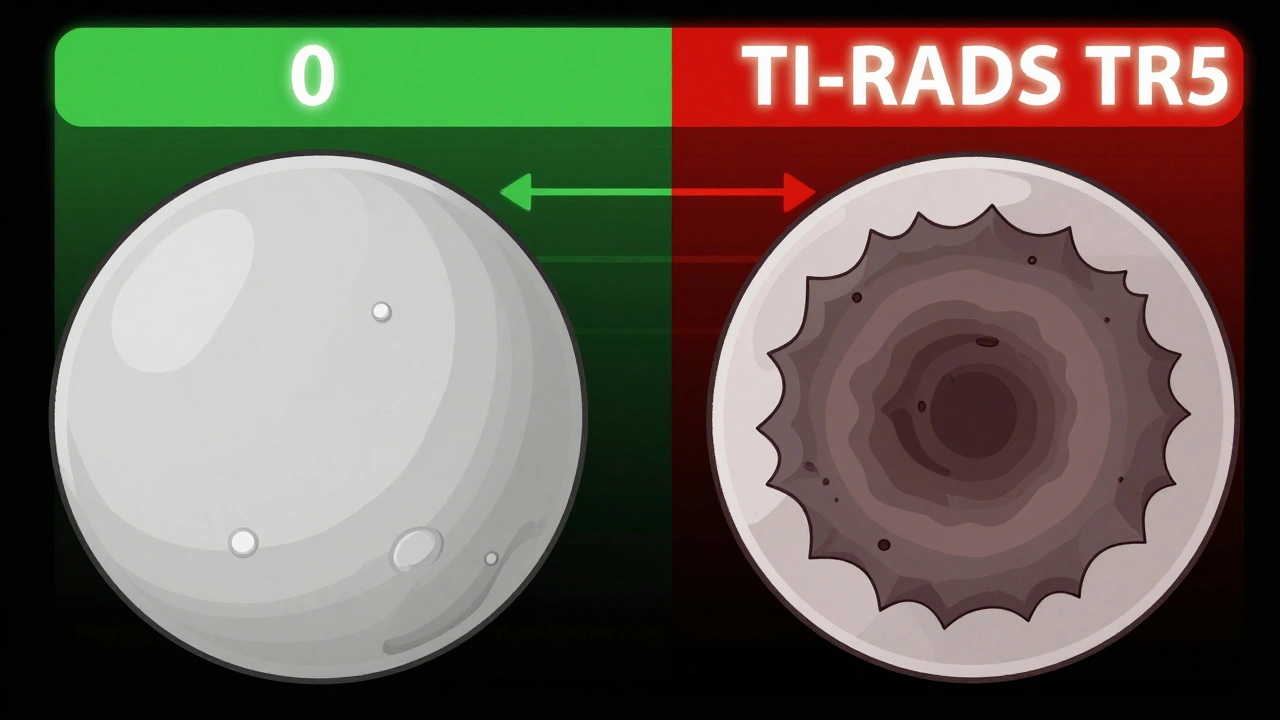
In 2017, the American College of Radiology created TI-RADS-a simple scoring system that turns what looks like a blurry picture into a clear risk level. Every nodule gets points based on five features:
Each feature gets 0 to 3 points. Add them up, and you get a TI-RADS category:
This system replaced older, less consistent guidelines. Studies show TI-RADS predicts cancer risk better than anything before it. And it’s now the standard in hospitals across the U.S., Europe, and beyond.
You might wonder: why not just do a CT scan or MRI? Or a nuclear thyroid scan?
CT and MRI can show a nodule if it’s big enough, but they can’t see the fine details-like microcalcifications or shape-that matter most. Nuclear scans tell you if a nodule is “hot” (overactive) or “cold” (underactive). Hot nodules almost never turn cancerous. Cold ones have about a 15% chance. But here’s the catch: a nuclear scan can’t tell you which cold nodule is the dangerous one. It just gives you a broad category.
Ultrasound is the only test that shows you the exact structure of the nodule. And it’s the only one that can guide a needle during a biopsy. That’s huge. Without ultrasound, biopsies miss the target nearly 25% of the time. With ultrasound guidance, that drops to under 5%.
It’s also cheaper-around $200 to $500 in the U.S.-and safer. No radiation. No needles. No waiting days for results. You walk in, lie back, and walk out with answers in 15 minutes.
Not every nodule needs a biopsy. Size matters, but so does appearance.
If a nodule is under 5 millimeters-even if it looks suspicious-you don’t need to do anything right away. The chance it’s cancerous is so low that watching it is safer than poking it.
For nodules 1 centimeter or larger with TR4 or TR5 features, biopsy is standard. For TR3 nodules (4.8% risk), biopsy is usually recommended if they’re 2.5 centimeters or bigger. Why 2.5 cm? Because studies show thyroid cancers smaller than that almost never spread or cause harm. You can safely watch them for years.
And here’s something surprising: not every cancer needs surgery. For tiny, low-risk papillary cancers under 1 cm, many doctors now recommend active surveillance-meaning regular ultrasounds every 6 to 12 months-instead of immediate removal. The 10-year survival rate is over 99%. Surgery comes with risks: nerve damage, voice changes, lifelong hormone replacement. If you don’t need it, why do it?
Ultrasound is powerful-but it’s not perfect. It can’t tell you for sure if a nodule is cancerous. Only a biopsy can do that.
Some nodules look suspicious but turn out benign. Others look harmless but turn out to be cancer. That’s why even with a perfect ultrasound, some results are indeterminate. About 15-30% of biopsies fall into this gray zone. That’s where molecular testing comes in. New gene tests can analyze the nodule’s DNA and say: “This is almost certainly benign” or “This has a high chance of being cancer.” These tests have cut unnecessary surgeries by half.
But even if the molecular test says “benign,” you still need follow-up ultrasounds. Cancer can grow slowly. And ultrasound is the tool that catches it early.
Not every ultrasound is created equal. The person holding the transducer matters. So does the machine.
Experts say it takes 200 to 300 supervised scans before a sonographer can reliably spot the subtle signs of cancer. Many community clinics don’t have that level of experience. Audits show that 35% of ultrasounds done outside major hospitals miss checking the lymph nodes in the neck-a critical part of cancer staging.
Good ultrasound machines need high-frequency probes (at least 10 MHz), Doppler to check blood flow, and compound imaging to sharpen the picture. If your clinic uses an old machine or the tech is rushed, you might get a false sense of security.
That’s why accreditation matters. Facilities with AIUM (American Institute of Ultrasound in Medicine) certification have proven they get 90% of nodule assessments right. Ask your doctor: “Is this facility accredited for thyroid ultrasound?”
Artificial intelligence is starting to change thyroid ultrasound. A 2023 study in Nature Scientific Reports showed a new AI model that looks at nodule shape, texture, and blood flow patterns. It got 94.2% accuracy-better than most human radiologists.
These tools don’t replace doctors. They help. They flag the tricky cases. They reduce mistakes. And they’re getting better fast.
Next up? Combining ultrasound features with genetic markers. Imagine a system that says: “Your nodule has a TR4 score, plus this specific gene mutation-that means your cancer risk is 42%.” That’s not science fiction. Researchers at Boston University and Dana-Farber are already testing it. Within five years, personalized risk scores could cut unnecessary biopsies by 30%.
If you’ve been told you have a thyroid nodule:
Thyroid cancer is often slow-growing. You have time to make smart decisions. Ultrasound gives you the map. You just need to understand the signs.
No. It’s completely painless. You lie on your back with your neck slightly extended. A small amount of gel is applied to your skin, and the probe is gently moved over your neck. You might feel a little pressure, but no discomfort. The whole thing takes 15 to 20 minutes.
No. Ultrasound can only assess the likelihood of cancer based on nodule features. It identifies suspicious patterns, but only a biopsy-where a tiny sample is taken and examined under a microscope-can confirm cancer. Ultrasound’s job is to tell you which nodules need a biopsy.
It depends on your risk. For low-risk nodules (TR1 or TR2), no follow-up is needed. For TR3 nodules under 2.5 cm, repeat ultrasound in 12 to 24 months. For TR4 or TR5, follow-up every 6 to 12 months, or sooner if the nodule grows. If you’ve had a benign biopsy, you still need yearly scans for at least 5 years to make sure nothing changes.
No. In fact, most aren’t. Up to 68% of adults have thyroid nodules, but less than 10% are cancerous. The vast majority are harmless, fluid-filled cysts or benign growths. Size and ultrasound features matter more than presence alone. A tiny nodule with smooth edges and no calcifications is far less concerning than a large, solid one with jagged edges and microcalcifications.
Sometimes. If your nodule is small (under 1 cm) and you’re low-risk overall, your doctor may suggest monitoring with repeat ultrasounds instead of biopsy. If the nodule stays stable for two years, it’s almost certainly benign. For larger or higher-risk nodules, biopsy remains the standard. Molecular testing can also help avoid surgery if the results strongly suggest benignity.
12 Responses
It's wild how something so simple can tell you so much. I always thought ultrasounds were just for babies, never thought they could read your thyroid like a book. Makes you wonder what else we're missing out on with old-school medicine.
Oh please. TI-RADS is just corporate medicine’s way of turning human judgment into a checkbox game. You know what’s really suspicious? A doctor who won’t look you in the eye and say ‘I don’t know.’
MY THYROID IS A MYSTERY 🤯 I got a nodule last year and now I’m obsessed with every tiny bump on my neck. I Google it at 2am. I cry. I scream. I buy essential oils. 😭🙏 #ThyroidLife
Just want to say if you're scared about this stuff you're not alone. I had a TR4 nodule and thought I was dying. Turns out it was benign. The key is finding a good clinic and asking questions. Don't let fear make the call. You got this. 💪
So if I got a tiny nodule under 1cm and it's TR3... I just chill? No biopsy? No surgery? Like... really? My doctor said ‘watch and wait’ and I thought he was blowing me off. Turns out he might’ve been right. Mind blown. 🤯
...and yet, despite all this ‘evidence-based’ precision, 35% of community ultrasounds miss lymph node assessment. So we’re trusting a system that’s flawed, funded by corporations, and over-reliant on untrained technicians. And you call this medicine?
Get the scan. Ask about TI-RADS. Don’t panic. Watch it. Act if it changes. Simple.
This is so helpful. In Nigeria, most people don’t even know what a thyroid ultrasound is. We just wait until the lump gets big. Thank you for explaining this so clearly. I’ll share this with my family.
So let me get this straight… you’re telling me I can skip surgery for cancer if it’s tiny? And they just… watch it? Like a pet goldfish? 😏 I mean… if I had a cancer that moved slower than my ex’s text replies, I’d be okay with that too.
Actually, you're all missing the bigger picture. In India, we have a 20-year study from AIIMS Delhi showing that TR3 nodules under 2cm have a 0.7% malignancy rate when combined with serum TSH levels below 2.5, which is lower than the American threshold. Also, the 10 MHz probe requirement? That's only true for high-end machines-many rural centers use 7.5 MHz with 92% sensitivity when operated by trained sonographers. And don't get me started on molecular testing costs-$2000 in the US, $150 in Bangalore. So yes, TI-RADS is useful, but it's a Western construct that doesn't account for global disparities in imaging access, nutritional factors like iodine deficiency, or genetic polymorphisms in the RET gene that increase risk in South Asian populations. Also, AI models are trained on biased datasets-most are based on Caucasian populations. So unless you're a white American woman with no comorbidities, this whole system might not apply to you. And if you're not asking your radiologist about their inter-observer agreement rates, you're not doing due diligence. Also, have you checked your vitamin D levels? Low D is linked to thyroid nodules. And also, have you considered that stress causes cortisol spikes that alter thyroid function? So maybe your nodule is just your body screaming for a vacation. Also, I had one. It went away after I did yoga and stopped eating gluten. Just saying.
One cannot help but observe the alarming epistemological reductionism inherent in the TI-RADS paradigm: a phenomenological experience of bodily anomaly is reduced to a quantitative algorithm, thereby erasing the hermeneutic dimension of patient embodiment. One is left to wonder whether this mechanistic fetishization of imaging metrics constitutes a form of medical alienation, wherein the living body becomes a mere dataset for administrative triage. Is this not the apotheosis of late-capitalist healthcare?
People need to stop treating thyroid cancer like it’s a minor inconvenience. It’s cancer. Period. If your nodule has microcalcifications, jagged margins, and is hypoechoic-you don’t ‘watch and wait.’ You get it out. You don’t gamble with your life because some ‘active surveillance’ study says it’s ‘low-risk.’ What if you’re the 1%? What then? Your silence won’t save you. Surgery has risks? So does dying. And if you’re too scared to face it, that’s your problem-not mine.