Most people think COPD is just a smoker’s disease. But what if you never smoked - yet still struggle to breathe by your 30s or 40s? That’s the reality for thousands with alpha-1 antitrypsin deficiency (AATD), a hidden genetic condition that causes lung and liver damage long before most expect it. It’s not rare. It’s just rarely tested for.
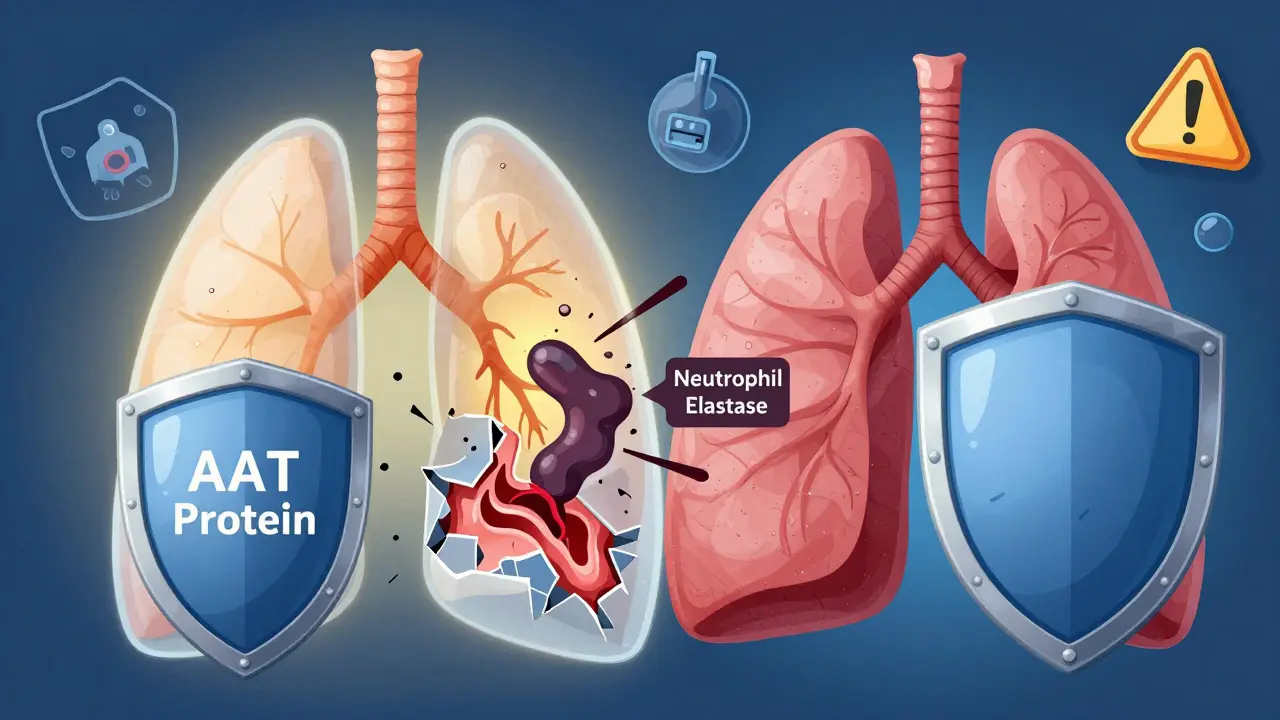
Alpha-1 antitrypsin (AAT) is a protein made in the liver. Its job? To protect your lungs from a destructive enzyme called neutrophil elastase. This enzyme normally fights infection, but without enough AAT to control it, the enzyme starts breaking down healthy lung tissue. The result? Early-onset emphysema - a type of COPD that hits people in their 30s and 40s, not their 60s.
The problem starts with a mutation in the SERPINA1 gene a gene on chromosome 14 that provides instructions for making the alpha-1 antitrypsin protein. Over 120 variants exist, but the Z and S alleles are the most dangerous. If you inherit two Z alleles (one from each parent), you have the ZZ genotype - the most severe form. Your liver produces misfolded AAT that gets stuck inside liver cells, and your bloodstream gets almost no protection. Serum levels drop to just 11-17 mg/dL - less than 20% of normal.
Most doctors don’t test for AATD unless you’re young, have no smoking history, or have liver problems. That’s a problem because symptoms look just like regular COPD: chronic cough, wheezing, shortness of breath, and frequent lung infections. Patients often go to three or more doctors over eight years before someone says, “Have you been tested for alpha-1?”
Studies show up to 3% of all COPD cases are actually AATD. That’s tens of thousands of people in the U.S. alone who are being treated for asthma or smoking-related COPD - while their real cause goes unaddressed. The American Lung Association estimates only 10% of those with severe AATD have been diagnosed. The rest are flying blind.
Smoking-related COPD usually shows up after age 60, with damage mostly in the upper lungs. AATD-related emphysema hits earlier - often before 45 - and hits the lower lungs hardest. On a chest scan, you’ll see the bottom lobes eaten away, not the top. This pattern is a red flag.
Another key difference: AATD can also wreck your liver. The same misfolded protein that’s missing from your blood builds up in your liver cells. This can cause cirrhosis, liver failure, or even liver cancer - even in children. About 10-15% of ZZ individuals develop liver disease by adulthood. That’s something you won’t see in typical COPD.

Testing is simple. First, a blood test checks your AAT level. If it’s below 50 mg/dL, you need genotyping. That tells you if you have ZZ, SZ, or another variant. Phenotyping (isoelectric focusing) can also identify the exact protein type.
The American Thoracic Society and European Respiratory Society say: Test everyone with COPD, asthma with fixed airflow blockage, unexplained liver disease, or a family history of AATD. Yet most don’t. Insurance often won’t cover it unless you’ve already been misdiagnosed for years.
The whole process - from first symptoms to diagnosis - can take 5 to 10 years. Many patients describe it as a “diagnostic odyssey.” One Reddit user wrote: “I was told I had asthma for 12 years. When they finally tested me, I had ZZ. My lungs were already half gone.”
There’s no cure. But there are ways to slow it down.
Augmentation therapy is the only treatment proven to slow lung damage. It’s weekly IV infusions of purified human AAT. Products like Prolastin-C, Zemaira, and Aralast NP raise your blood levels above 11 μM - the minimum needed to protect your lungs. Studies show this can reduce lung function decline by up to 60% over 5 years.
But it’s not perfect. It doesn’t help your liver. It doesn’t reverse damage. And it costs $70,000-$100,000 a year. Insurance denies nearly half of initial claims. Many patients spend months appealing - or pay out of pocket.
There’s a new option: Kedrab the first subcutaneous AAT therapy approved by the FDA in 2022. Instead of IV infusions every week, you give yourself a shot under the skin. It’s less time-consuming, less painful, and more convenient. It’s not yet widely available, but it’s a major step forward.
For liver damage, the only option is a transplant - if you get to that point. That’s why stopping smoking is non-negotiable. If you have ZZ and smoke, your risk of severe emphysema jumps 75%. Quitting can cut that risk by 60%. One patient on PatientsLikeMe said: “I quit smoking the day I got my diagnosis. I’m 52 now. I still hike. My doctor says I owe it to quitting.”
Researchers are working on therapies that target the root cause - not just the symptoms.
Small molecule drugs are being tested to stop the misfolded AAT from clumping in the liver. RNA interference (RNAi) therapies aim to silence the faulty gene, reducing toxic protein buildup. Gene therapy trials are starting too - one using CRISPR to fix the mutation in liver cells.
Newborn screening is expanding. Twelve U.S. states now test for AATD as part of routine newborn panels. That means kids with ZZ can be monitored from birth - and protected before lung damage starts. This could change everything.

If you have COPD - especially if you’re under 45, never smoked, or have a family history - get tested. Ask your doctor for an AAT level test. If it’s low, push for genotyping.
If you’re diagnosed:
Don’t wait for a crisis. AATD is silent until it’s too late. But with early detection and the right care, you can live a long, active life.
Weekly IV infusions are exhausting. Finding a vein after years of treatment can be painful. Missed work. Travel disruptions. Insurance battles. These aren’t side effects - they’re daily realities.
But support exists. The Alpha-1 Foundation connects patients with resources, advocacy, and clinical trial updates. Online communities like Alpha-1 Community offer peer advice - not just medical facts.
One woman in Ohio, diagnosed at 38, started a local support group. “We share infusion tips. We fight insurance denials together. We remind each other: this isn’t just a lung disease. It’s a family disease.”
No. Alpha-1 antitrypsin deficiency (AATD) is a genetic disorder that can cause COPD - specifically early-onset emphysema. Most COPD is from smoking or air pollution. AATD is a specific, inherited cause that affects only about 3% of COPD patients. But if you have AATD and smoke, your COPD will develop faster and worse than in someone without the gene.
Yes - but only if both parents carry a faulty gene without knowing it. AATD is inherited in an autosomal codominant pattern. You need two bad copies (like ZZ or SZ) to have severe disease. Many people carry one copy (like MZ) and never show symptoms. They can pass it on. That’s why family history matters - even if no one in your family has been diagnosed.
No. Augmentation therapy replaces AAT in the bloodstream to protect the lungs, but it doesn’t clear the misfolded protein stuck in the liver. Liver damage from AATD needs separate monitoring. In severe cases, a liver transplant may be the only option. Researchers are testing drugs that target liver buildup directly - but none are approved yet.
Often, yes - if you have COPD, unexplained liver disease, or a family history. Most insurers cover the initial AAT level test. Genotyping is usually covered too, but you may need a letter from your doctor explaining why. Some patients face denials, especially if they’re young or non-smokers. Appeals are common. Patient advocacy groups like the Alpha-1 Foundation offer help with insurance paperwork.
Absolutely - if you act early. Many people with ZZ genotype live into their 70s and 80s. Key factors: never smoking, getting augmentation therapy if eligible, regular lung and liver monitoring, and staying active. One man in his 60s, diagnosed at 39, runs marathons. His secret? “I quit smoking. I got treated. I didn’t wait.”
AATD isn’t just another lung disease. It’s a genetic puzzle piece that, when found, changes everything. It means your COPD isn’t your fault. It means your family might be at risk. It means there’s a treatment - not just for symptoms, but for the root cause.
The biggest mistake? Waiting. The biggest win? Getting tested. If you’ve been told you have COPD - and you’re under 45, never smoked, or have liver issues - don’t assume. Ask. Push. Demand the test. Because for AATD, early detection isn’t just helpful - it’s life-changing.
14 Responses
I was diagnosed with ZZ at 34. They told me I had asthma for six years. Six years. My lungs are shot now. I don't blame the doctors. I blame the system. No one tests for this unless you're already on oxygen. And even then, they act like you're asking for a miracle. This isn't rare. It's ignored. And people are dying because no one wants to admit it's genetic.
So let me get this straight. The same protein that's supposed to protect your lungs is also secretly poisoning your liver? And we're giving people weekly IVs of purified human protein like it's some kind of vampire blood transfusion? Meanwhile, Big Pharma is charging $100k a year to keep you alive while they sit on gene therapies that could fix this permanently. Of course. Because capitalism doesn't care if your lungs are being eaten by your own genetics.
The epidemiological data is fundamentally flawed. The 3% figure is pulled from retrospective cohorts with selection bias. Most AATD cases are never genotyped because the screening protocols are outdated. The real prevalence is likely 7-12% among early-onset COPD populations. We're underestimating the burden because we're using 1990s diagnostic criteria in a 2024 genomic era. Also, liver involvement is underreported because hepatologists don't screen for AATD unless there's cirrhosis. That's not clinical diligence. That's negligence.
I know someone who got diagnosed after her 5-year-old had liver failure. Turns out Mom had ZZ. No one tested her. No one tested her dad. No one tested her sister. Now they're all on augmentation therapy. But the insurance company denied her first claim because "it's not medically necessary for a non-smoker." Non-smoker? My god. It's genetic. It's not a lifestyle choice. It's not a moral failing. It's a mutation. And we're treating it like a personal failure.
You ever try to explain to a 60-year-old insurance adjuster that your lungs are being shredded by your own damn DNA? I have. I sat in a call center for 47 minutes while they asked me if I "ever used a vape." I didn't even know what a vape was until last year. I'm 39. My dad died of liver cancer at 51. My brother has emphysema. We're not outliers. We're the rule. And the system treats us like we're lying to get free drugs.
I got my diagnosis in 2021. I was 31. I had been on albuterol since I was 17. My doctor said I was "just sensitive." I didn't know what AATD was. I didn't know my dad had it. He died at 54. They called it "emphysema." No one said "genetic." I wish someone had. I wish someone had just asked.
I just got my first infusion yesterday. Took 3 hours. I had to drive 90 miles. My vein collapsed. I cried. I didn't want to. But I'm alive. I'm 42. I still work. I still hike. I still laugh. I'm not a statistic. I'm not a case study. I'm here. And I'm fighting. And if you're reading this and you're undiagnosed? Get tested. Don't wait. Don't be scared. Just go.
In India, this is almost unheard of. No screening. No awareness. I work in a pulmonology clinic. Last month, a 36-year-old came in with severe emphysema. Never smoked. We tested him. ZZ. His brother had the same. His mother had liver cirrhosis at 48. We told him to get his kids tested. He looked at me like I was speaking alien. "Why? We are not sick." This is the silent epidemic. No one knows. No one cares.
I’ve been on augmentation for seven years. I’ve lost three friends to liver failure. I’ve watched one guy go from hiking the Rockies to needing oxygen just to shower. I’ve sat in hospital waiting rooms while nurses argued over whether my IV line was "medically necessary." I’ve had my insurance cancel my coverage three times. I’ve had to sleep in my car outside the infusion center because I couldn’t afford the parking. This isn’t medicine. This is a war. And we’re the ones getting shot.
I’m not saying this isn’t real. But let’s be honest. If you’re getting weekly infusions and you’re not a billionaire, you’re either rich or you’re on a government program. And if you’re on a government program, you’re probably on Medicaid. And if you’re on Medicaid, you’re probably not getting the new subcutaneous stuff. You’re getting the old IV stuff. And it’s not working as well. So yeah. You’re alive. But you’re not living.
I just got my genotyping results. I’m MZ. My mom was ZZ. I never had symptoms. I’m 28. Should I be worried? My kids? My wife? I read that MZ carriers have a slightly higher risk of lung disease if they smoke. But what if I don’t smoke? What if I never will? Is there any long-term data? I’m not asking for a diagnosis. I’m asking for clarity.
You think this is about lungs? No. It’s about control. The system doesn’t want you to know this is genetic. Because if it is, then it’s not your fault. And if it’s not your fault, then who do you blame? The doctors? The insurance companies? The government? The pharmaceutical companies? No. You blame yourself. And that’s easier. So they keep testing for smoking. Keep calling it asthma. Keep telling you to lose weight. Keep telling you to quit. But you didn’t start this. Your genes did. And they’re not asking for your permission.
I'm 41. ZZ. On Kedrab now. Shot every 2 weeks. No more IVs. No more vein trauma. I can do it at home. I can sleep. I can work. I can travel. I can breathe. I'm not cured. But I'm not dying. And I'm not alone. There are thousands of us. We're not broken. We're just misunderstood. And now? We're fighting back.
I’ve been researching this for years. The science is solid. The genetics are clear. The treatment works. The problem is access. Not awareness. Not knowledge. Access. In rural America, there are 12 infusion centers for a population of 30 million. In Australia, it’s better - but still not universal. In developing countries? Forget it. This isn’t a medical issue. It’s a distribution problem. We have the cure. We just won’t deliver it to the people who need it most. And that’s not negligence. That’s choice.