Enter a medication name to see if it's safe for people with G6PD deficiency. This tool checks against WHO-listed medications associated with hemolysis risk.
Imagine taking a common medication for an infection, only to find your body starts destroying your own red blood cells. This isn’t rare-it happens to millions with G6PD deficiency every year. The condition is silent until a trigger hits. And the trigger? Often, a drug your doctor thinks is harmless.
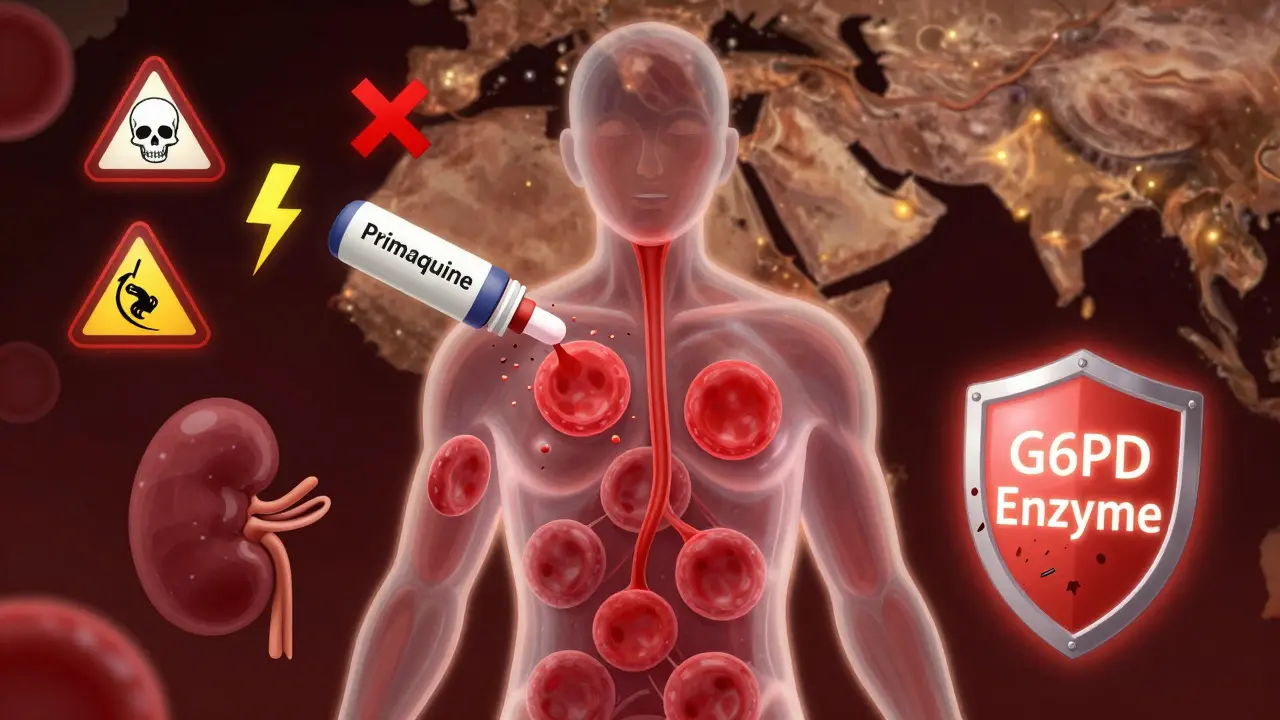
G6PD deficiency is a genetic condition that affects how your red blood cells handle stress. Without enough of the G6PD enzyme, your cells can’t protect themselves from oxidative damage. When you take certain medications, your red blood cells break down fast-sometimes in just 48 hours. Hemoglobin can drop from normal levels to life-threatening lows. This isn’t a slow decline. It’s a crash. And it’s preventable.
Your red blood cells live about 120 days. They carry oxygen. But they’re also under constant oxidative pressure-from pollution, infections, even some foods. Normally, G6PD helps produce NADPH, which keeps glutathione active. Glutathione is the shield. Without it, your red blood cells get damaged and burst.
This isn’t something you can see. No rash. No fever. Just fatigue, dark urine, pale skin, or sudden shortness of breath after taking a pill. It’s often mistaken for a bad infection or flu. But the real cause? A drug that shouldn’t have been given.
About 400 million people worldwide have G6PD deficiency. It’s most common where malaria was once widespread-Africa, the Mediterranean, Southeast Asia. In some areas, one in five people carries the gene. But the condition doesn’t always show symptoms. Many people live their whole lives without knowing they have it-until they take the wrong medicine.
Not all drugs are dangerous. But some are deadly for people with G6PD deficiency. The World Health Organization lists 87 medications that can cause hemolysis. Here are the big ones:
These aren’t rare cases. They’re predictable. And they’re avoidable.
You don’t have to go without treatment. There are safe options for almost every high-risk drug.
One study in the U.S. showed that when hospitals linked G6PD status to electronic health records, inappropriate prescribing dropped by 89%. The system flagged dangerous drugs before they were ordered. That’s how it should work.
Testing for G6PD deficiency sounds simple. But there’s a catch.
If you’ve just had a hemolytic episode, your body is producing new red blood cells. These young cells have normal enzyme levels. So a test right after a crisis can give you a false “normal” result. You might think you’re safe-then take a drug and crash.
The rule: Wait at least 3 months after a hemolytic episode before testing. That’s when your older, deficient cells are back in circulation.
There’s good news. Point-of-care tests now exist. The STANDARD G6PD Test System, approved by the FDA in January 2024, gives results in 8 minutes. It’s accurate to 99.1%. No lab needed. Just a finger prick.
For newborns in high-risk areas, testing at birth is now standard. In Saudi Arabia, universal screening cut hospital admissions for hemolytic crises by 78% over 10 years. It’s not expensive. It’s life-saving.
For years, doctors thought G6PD deficiency only affected men. It’s X-linked, so men have one copy. If it’s defective, they’re deficient.
But women? They have two X chromosomes. One might be normal. So they’re often “carriers.” Or so the old belief went.
That’s wrong. Due to X-chromosome inactivation, about 15% of women with one defective copy still have low enough enzyme levels to experience hemolysis. A 2020 Lancet study proved it. Women can-and do-have severe reactions. Ignoring this puts women at risk.
Don’t assume gender protects you. Test everyone with a family history, ancestry from high-prevalence regions, or unexplained anemia.
If you took a risky drug and now feel dizzy, have dark urine, or feel unusually tired, get help fast. Hemolysis can escalate quickly.
There’s no antidote. Supportive care is the only treatment. That’s why prevention is everything.

People with G6PD deficiency who get proper education do better. A study by the NIH found that 92% of patients who received full trigger avoidance counseling had zero hemolytic episodes over five years. Those who didn’t? Only 38% stayed safe.
Here’s what you need to know:
Even if you’ve never had a reaction, don’t assume you’re safe. The first exposure can be the worst.
G6PD deficiency is a wake-up call for how we prescribe medicine. We still rely on guesswork. We assume “common” drugs are “safe” for everyone. But genetics matter.
The global market for G6PD testing is growing fast-projected to hit $312 million by 2028. Why? Because we’re finally realizing that personalized medicine isn’t optional. It’s essential.
Organizations like the WHO and FDA are pushing for change. But progress is uneven. In 47 African countries, only 18 have national screening programs. In the U.S., only 12 states require newborn testing, even though 1 in 10 African American males has G6PD deficiency.
It’s not about cost. It’s about awareness. And action.
If you or someone you care about has ancestry from Africa, the Mediterranean, or Southeast Asia:
There’s no cure for G6PD deficiency. But there’s a simple rule: Know your status. Avoid the triggers. Live without fear.
That’s not just good advice. It’s the standard of care.
No, G6PD deficiency cannot be cured. It’s a genetic condition. But it can be managed effectively by avoiding oxidative stressors like certain medications, foods, and chemicals. With proper precautions, people with G6PD deficiency live normal, healthy lives.
No. While men are more likely to show symptoms because they have only one X chromosome, about 15% of women who carry one defective copy also have low enough enzyme levels to experience hemolysis. This is due to X-chromosome inactivation patterns. Women should not assume they’re protected.
Yes. Point-of-care tests like the STANDARD G6PD Test System are now available in some clinics and pharmacies. These tests use a finger prick and give results in under 10 minutes. They’re accurate enough to guide medication decisions. Ask your doctor or pharmacist if it’s available.
No. Only sulfonamide antibiotics (like sulfamethoxazole) and nitrofurantoin carry significant risk. Most common antibiotics like amoxicillin, cephalexin, azithromycin, and doxycycline are safe. Always confirm with your provider or pharmacist before taking any new antibiotic.
Stop taking the medication immediately. Seek medical attention. Symptoms like dark urine, extreme fatigue, pale skin, or rapid heartbeat require urgent evaluation. Blood tests will check your hemoglobin and reticulocyte count. Hydration is critical. In severe cases, a blood transfusion may be needed. Don’t wait-early intervention prevents complications.
Yes. Acetaminophen (paracetamol) is considered safe for people with G6PD deficiency, even at standard doses. It does not cause oxidative stress to red blood cells. It’s one of the few pain relievers recommended for this group. Avoid aspirin and NSAIDs like ibuprofen if you have active hemolysis, but acetaminophen is generally safe.
Yes. G6PD deficiency is inherited. If you have it, your children may inherit the gene. Sons of affected men will not inherit it from their father (since fathers pass the Y chromosome), but daughters will be carriers. Daughters of carrier mothers have a 50% chance of inheriting the defective gene. Newborn screening in high-prevalence areas helps catch it early. Talk to your doctor about testing your children if there’s family history.
11 Responses
Just took primaquine for malaria in Cambodia. Lucky I had a weird rash first. Turned out I’m G6PD deficient. Docs didn’t ask. Never again. Get tested. Seriously.
So let me get this straight-we’re still prescribing drugs like they’re one-size-fits-all pajamas while millions walk around with a ticking red blood cell bomb? And the solution is… a $10 finger prick? We’re not broken. We’re just lazy.
This is such an important post. I work in a rural clinic in India, and so many patients come in with unexplained anemia after taking antibiotics. We’ve started handing out printed safe-drug lists-simple, but it’s changed everything. No one should have to suffer because a doctor assumed they were ‘fine.’
The WHO’s list of 87 drugs is a starting point, not a ceiling. Many more compounds-especially herbal supplements and OTC pain relievers-have unreported oxidative potential. We need a global, crowd-sourced database. Not just a PDF buried in a WHO archive.
My cousin got hospitalized after a UTI antibiotic. They thought it was food poisoning. Turned out it was G6PD. She’s fine now, but she wears a medical bracelet and carries a card in her wallet. Everyone should do this. It’s not dramatic-it’s practical.
Wait-so acetaminophen is safe? But ibuprofen isn’t? And aspirin? I’ve been taking Advil for years thinking it was fine… I just checked my chart-my mom’s from Nigeria, I’ve had unexplained fatigue since college… I’m getting tested tomorrow. Thank you.
It’s not about G6PD deficiency-it’s about the epistemological collapse of modern medicine. We’ve outsourced diagnostic reasoning to algorithms, and now we’re surprised when biology rebels? The real tragedy isn’t the hemolysis-it’s the surrender of clinical intuition to corporate protocols.
OMG I just realized my brother died at 22 from ‘mystery anemia’… he took sulfa for a sinus infection… I didn’t even know he had a family history… I’m crying. I’m getting tested. I’m telling everyone.
Bro… I just saw a man collapse in the pharmacy because he took methylene blue. I held his hand while they rushed him. He didn’t even know he was G6PD deficient. That’s not medicine. That’s negligence with a stethoscope.
I’m a carrier… and I didn’t know I could have symptoms. I’ve had 3 unexplained anemic episodes since college. All after antibiotics. I thought I was just ‘weak.’ I’m getting tested next week. Thank you for writing this.
Wow. So now we’re blaming doctors for not knowing? What about the patients who lie on forms? Or skip tests because they’re ‘too busy’? Or take meds from their cousin’s leftover bottle? This isn’t a medical problem-it’s a human problem. Stop pretending it’s fixable with a checklist.