
This tool helps you assess your risk of hypoglycemia (low blood sugar) based on your specific sulfonylurea medication, age, dose, and other factors. Results are personalized and indicate whether you should discuss options with your doctor.
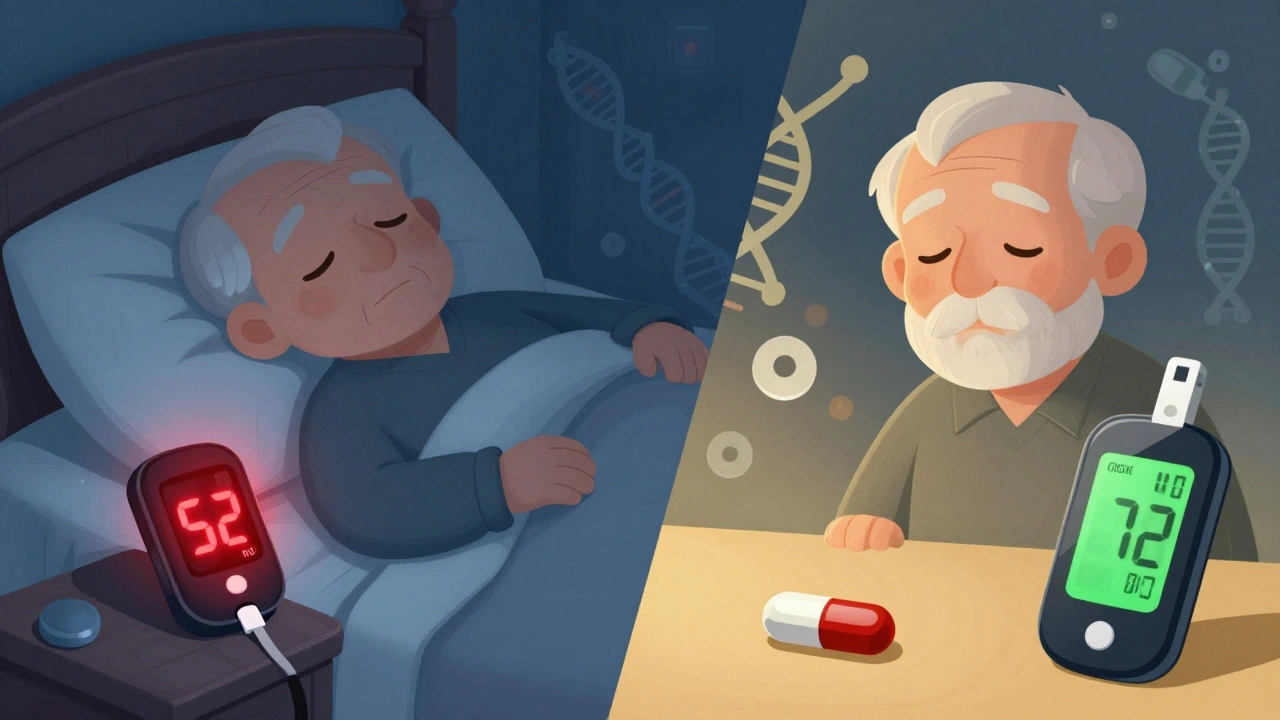
When you're managing type 2 diabetes, taking a pill that lowers your blood sugar seems like a good thing-until your blood sugar drops too low. That’s the real risk with sulfonylureas, one of the oldest and still widely used classes of diabetes medications. These drugs work by forcing your pancreas to release more insulin, no matter how low your blood sugar already is. That’s why hypoglycemia-dangerously low blood sugar-isn’t just a side effect. It’s an expected outcome for many people taking them.
Sulfonylureas don’t wait for your body to signal that it needs insulin. They override the natural system. Once you take them, they bind to receptors on your pancreatic beta cells and trigger insulin release-whether your blood sugar is 80 mg/dL or 180 mg/dL. That’s why even skipping a meal or going for a walk after taking your pill can send your glucose crashing.
The most common sulfonylureas in the U.S. are glyburide, glipizide, and glimepiride. Of these, glyburide is the biggest culprit. It’s long-acting, stays in your system for up to 10 hours, and has active metabolites that keep working even after the original dose wears off. That’s why so many people report midnight lows or sudden dizziness after lunch. Glipizide and glimepiride, on the other hand, are shorter-acting and clear faster. Studies show glipizide causes about 30-40% fewer hypoglycemic episodes than glyburide.
Even the dose matters. A 2023 study in Diabetes Care found that people taking glyburide at 10 mg or higher had nearly triple the risk of severe hypoglycemia compared to those on 5 mg or less. Yet, many doctors still start patients on 5 mg or even 10 mg daily-way above the recommended starting dose of 1.25-2.5 mg.
It’s not just about the drug. Your age, other medications, and genetics all play a role.
If you’re over 65, your risk jumps. The American Geriatrics Society specifically warns against glyburide in older adults because it increases hypoglycemia risk by 2.5 times compared to glipizide. Older bodies clear drugs slower, have less muscle mass to store glucose, and often have blunted warning signs-like not feeling shaky or sweaty when blood sugar drops.
Other drugs can make things worse. If you’re taking gemfibrozil (for cholesterol), sulfonamide antibiotics, or warfarin, they can push more sulfonylurea into your bloodstream by knocking it off protein binding sites. One study found gemfibrozil increases free glyburide levels by 30-40%, turning a safe dose into a dangerous one.
And then there’s your genes. About 15% of people carry a variant in the CYP2C9 gene (called *2 or *3) that slows how fast your body breaks down sulfonylureas. These people are 2.3 times more likely to have severe lows. Yet, almost no doctor orders a genetic test before prescribing these drugs.
Early signs are clear if you know what to look for:
These aren’t "just stress" or "getting old." They’re your body screaming for glucose. If you ignore them, you can slip into seizures, loss of consciousness, or even coma. People on sulfonylureas are 3 times more likely to end up in the ER for hypoglycemia than those on newer drugs like DPP-4 inhibitors or SGLT-2 blockers.
One Reddit user, "Type2Warrior87," wrote: "Switched from metformin to glyburide last month and have had 3 severe lows requiring glucagon-my doctor didn’t warn me this could happen multiple times per week." That’s not rare. A 2023 analysis of 1,247 posts on the American Diabetes Association’s forum showed 68% of sulfonylurea users had at least one low, and 22% had severe episodes needing help.
Prevention isn’t about being perfect. It’s about smart choices.
1. Start low, go slow. The ADA recommends starting glyburide at 1.25-2.5 mg and glipizide at 2.5-5 mg. Most patients don’t need more than 5 mg daily. Titrate up only if blood sugar stays high after 2-4 weeks.
2. Avoid glyburide if you can. Glipizide, glimepiride, and gliclazide (available outside the U.S.) are safer. If you’re on glyburide and having lows, ask your doctor about switching. One user on DiabetesDaily.com said: "After switching from glyburide to glipizide, my hypoglycemia dropped from weekly to once every 2-3 months."
3. Use a continuous glucose monitor (CGM). A 2022 trial called DIAMOND showed sulfonylurea users wearing CGMs had 48% less time spent in hypoglycemia. You don’t need to guess when you’re low-you’ll see it coming. Even basic CGMs alert you before your glucose hits 70 mg/dL.
4. Always carry fast-acting sugar. Keep glucose tablets, juice boxes, or candy in your bag, car, and bedside table. For mild lows, 15 grams of glucose is enough. Wait 15 minutes. Check again. Repeat if needed. Don’t eat a whole meal right away-overcorrecting causes rebound highs.
5. Watch for drug interactions. Tell every doctor you see-dentists, cardiologists, even your pharmacist-that you’re on a sulfonylurea. Avoid gemfibrozil, certain antibiotics, and NSAIDs like celecoxib if possible. If you must take them, your dose may need adjustment.
These drugs aren’t evil. They’re cheap-generic glipizide costs about $4 a month-and they lower A1C just as well as newer, pricier drugs. But they come with a trade-off: more lows.
If you’ve had two or more hypoglycemic episodes in six months, especially if you needed help or glucagon, it’s time to talk about alternatives. Newer options like GLP-1 receptor agonists (semaglutide, dulaglutide) or SGLT-2 inhibitors (empagliflozin, dapagliflozin) don’t cause lows and even protect your heart and kidneys. They’re more expensive, yes-but not if you’re in the ER every few months.
The ADA and EASD agree: sulfonylureas are still appropriate for some people, but only when risk is actively managed. That means choosing the right agent, using the lowest effective dose, avoiding them in older adults, and monitoring closely.

There’s new hope on the horizon. The PharmGKB now recommends testing for CYP2C9 variants before starting sulfonylureas. If you have the *2 or *3 allele, you might need only half the usual dose. An ongoing trial called RIGHT-2.0 is testing whether genotype-guided dosing can cut hypoglycemia by 40%. Early results are promising.
Another approach? Combine low-dose sulfonylureas with GLP-1 drugs. The DUAL VII trial showed this combo reduced hypoglycemia by 58% compared to sulfonylurea alone. You get the cost benefit of sulfonylureas with the safety of newer agents.
For now, the message is simple: if you’re on a sulfonylurea and you’re having lows, it’s not your fault. It’s the drug’s design. Talk to your doctor. Ask if you’re on the safest version. Ask if you need a CGM. Ask if there’s a better option. You don’t have to live with the fear of sudden lows.
No. Glyburide has the highest risk due to its long half-life and active metabolites. Glipizide, glimepiride, and gliclazide are shorter-acting and cause fewer lows-up to 40% fewer than glyburide. If you’re on glyburide and having frequent hypoglycemia, switching to glipizide is one of the most effective ways to reduce risk.
No. Stopping suddenly can cause your blood sugar to spike, especially if you’ve been taking them for months. Always talk to your doctor before making changes. They may recommend switching to a safer medication or adjusting your dose. Never discontinue without medical guidance.
Sulfonylureas force your pancreas to release insulin regardless of your blood sugar level. Even if you eat on time, your body may still produce too much insulin, especially if you’re on a high dose or a long-acting version like glyburide. Exercise, stress, or alcohol can also trigger lows even with regular meals.
Yes. The American Geriatrics Society’s Beers Criteria specifically advises against glyburide in adults over 65 because it doubles the risk of severe hypoglycemia. Glipizide is preferred because it’s shorter-acting, has no active metabolites, and clears faster from the body-making it much safer for older adults.
Yes. About 15% of people have CYP2C9 gene variants (*2 or *3) that slow how fast their body breaks down sulfonylureas. These people are over twice as likely to have severe hypoglycemia. Testing before starting the drug can help doctors choose a lower starting dose, reducing risk significantly. The PharmGKB now recommends this testing for all patients considering sulfonylureas.
Yes. Continuous glucose monitors (CGMs) are the most effective non-drug tool-they reduce hypoglycemia time by nearly half. Structured education on recognizing early symptoms and treating lows with 15g of glucose also cuts episodes by 32%. Avoiding alcohol on an empty stomach and keeping consistent meal timing helps too.
If you’re on a sulfonylurea and haven’t had a low yet, that’s good-but don’t assume you’re safe. Talk to your doctor about:
If you’ve had a low, especially one that required help or glucagon, it’s time to reassess. The goal isn’t just to control your A1C-it’s to live without fear. There are safer, just-as-effective options out there. You deserve both control and peace of mind.
14 Responses
Ugh, another post about sulfonylureas. I get it, they’re risky. Can we just move on to newer meds already? 🙄
i swear i thought i was just tired until my glucose monitor went off at 4am. now i know it was glyburide. thanks for the clarity 😅
For anyone on glyburide and having lows - switch to glipizide. Seriously. I switched last year and my hypoglycemic episodes dropped from 3x a week to maybe once a month. Also, get a CGM even if you’re not on insulin. It’s life changing. No hype, just facts. Your future self will thank you.
And yes, your doctor probably didn’t tell you this because they’re stuck in 2005. Don’t wait for them to catch up.
The CYP2C9 genetic variant data is underutilized but critical. In clinical practice, we’ve seen patients on standard glyburide doses with *3 alleles crash into severe hypoglycemia within days. Pharmacogenomic testing isn’t luxury - it’s preventative medicine. The ADA guidelines mention it, but insurance rarely covers it. That’s the real problem.
Also, glimepiride’s metabolites are less problematic than glyburide’s. If glipizide isn’t available, it’s the next best option. Gliclazide? Even better - if you can get it.
Let’s be real - doctors prescribe glyburide because it’s cheap and they don’t care enough to look up the guidelines. I’ve seen 70-year-olds on 10mg daily because the rep gave them free samples. This isn’t medical negligence - it’s systemic laziness. And now people are dying from preventable lows.
Stop blaming patients for not eating enough. The drug is the problem. Not their lifestyle. Not their discipline. The drug. End of story.
So you’re telling me I’ve been scared of my own body for years… because a pill was designed in the 1950s? 😂
At least now I know it’s not me. It’s the damn drug. Thanks for the validation.
Have you ever wondered why Big Pharma still pushes sulfonylureas? Because they’re generic. No patent. No profit. But wait - they’re not pushing them… the doctors are. And why? Because the FDA didn’t ban them. And why didn’t they? Because the lobbyists didn’t care enough. And why didn’t the lobbyists care? Because the patients didn’t scream loud enough.
It’s not about medicine. It’s about power. And someone’s making money off your fear.
PS: I once saw a guy pass out in a Walmart aisle because his glyburide didn’t wear off. He had no CGM. No glucagon. Just a $4 pill and a prayer. This isn’t healthcare. It’s a gamble.
If you’re not questioning why we still use drugs that override your body’s natural feedback loops, you’re not thinking deeply enough. Insulin isn’t a valve to be forced open - it’s a symphony. Sulfonylureas are a jackhammer in the orchestra.
We treat diabetes like a math problem. But the body isn’t a spreadsheet. It’s a living, breathing, evolving system. And we’re treating it like a broken toaster.
Maybe the real cure isn’t a new drug. Maybe it’s humility.
Ugh. I read this entire thing. And I’m still not convinced glipizide is better. I mean, it’s just another sulfonylurea. Why not just go straight to semaglutide? It’s not like the cost is astronomical anymore. I’m just saying… if you’re gonna make a change, make a *real* change.
Also, CGMs are overrated. My friend’s cousin’s neighbor got one and it just made them paranoid. 😒
Why are we even talking about this? In America, we’ve got better options. If you’re still on glyburide, you’re probably getting your meds from some Indian pharmacy that doesn’t even know what a CGM is. 🇺🇸💪
Stop being lazy. Switch. Or move to Canada. They don’t do this crap there.
Everyone’s acting like this is news. I’ve been on glimepiride for 8 years. No lows. No drama. The problem isn’t the drug class - it’s the idiots prescribing 10mg glyburide to 80-year-olds with kidney issues. This isn’t science. It’s criminal negligence wrapped in a white coat.
Also, stop romanticizing CGMs. They’re expensive. They beep. They lie. I’ve had 3 false alarms in one night. I’d rather just eat a banana and move on.
It is not merely a pharmacological issue, but an epistemological one - we have allowed mechanistic reductionism to dominate our therapeutic paradigms, wherein the human organism is reduced to a biochemical algorithm, and insulin secretion is treated as a binary switch rather than a dynamic, homeostatic equilibrium. The sulfonylurea, in its crude insistence upon insulin release irrespective of metabolic context, embodies the arrogance of 20th-century medicine - a relic of an era when we believed we could command biology without understanding its poetry.
Perhaps, then, the true path to healing lies not in substituting one molecule for another, but in restoring the patient’s agency - in listening, in observing, in respecting the body’s innate wisdom, rather than overriding it with pharmacological fiat. The real question is not whether glipizide is safer - but whether we are worthy of being entrusted with such power.
My uncle in Delhi was on glyburide for 10 years. He had 4 hypoglycemic episodes, one time he fell and broke his hip. We switched him to glimepiride and now he’s fine. No more midnight crashes. Just a simple change. No fancy gadgets. Just better medicine.
Don’t overcomplicate it. If you’re having lows, ask your doctor about switching. It’s that easy.
Just got my CGM last week. First night it alerted me at 58. I ate 3 glucose tabs. 15 mins later - 92. I cried. Not because I was low - because I finally felt safe. 🥲❤️
Also, my doc didn’t know about CYP2C9. I had to Google it and bring the paper. He changed my dose. I’m not mad. I’m just… glad I didn’t give up.