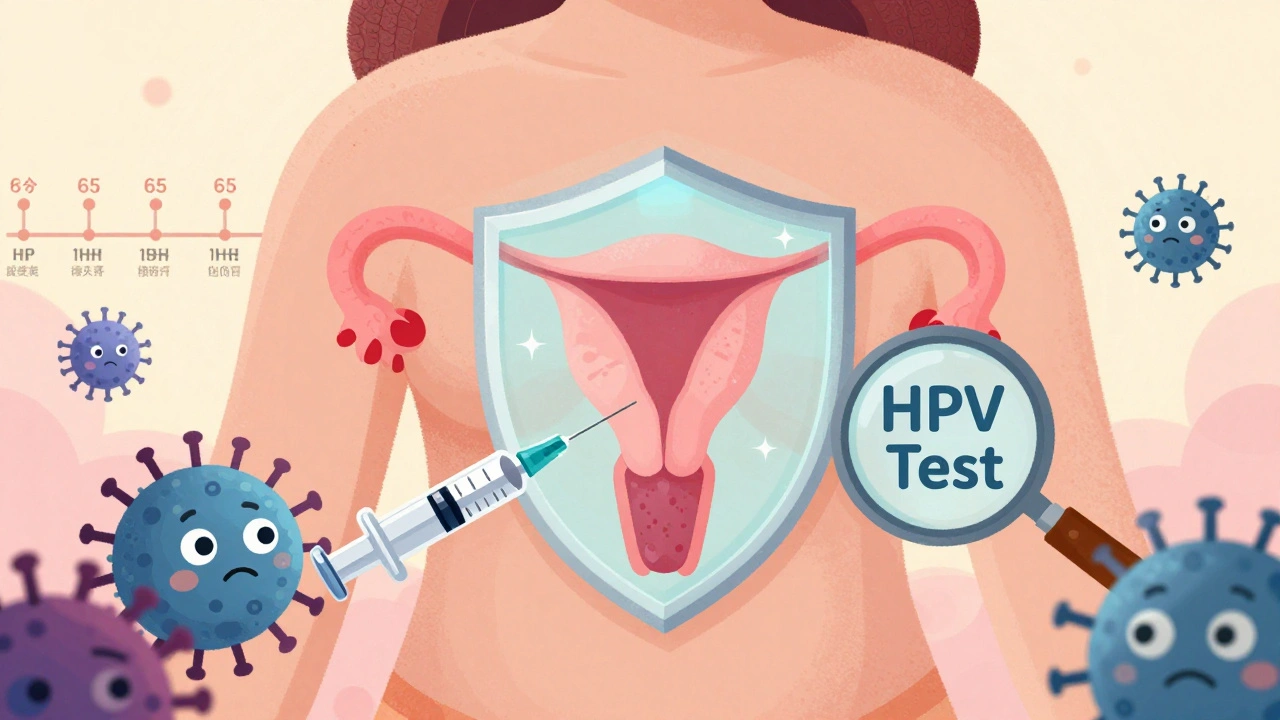
When you hear HPV testing, a medical procedure used to detect human papillomavirus infections that can lead to cervical cancer. Also known as HPV DNA test, it’s now a standard part of women’s health checkups — and sometimes for men too, depending on risk factors. Unlike the Pap smear, which looks for abnormal cells, HPV testing finds the virus itself. That means it can spot trouble years before changes show up on a Pap test.
Most people get HPV at some point in their lives — it’s that common. But not all types are dangerous. Only a few high-risk strains, like HPV 16 and 18, are linked to cancer. That’s why testing doesn’t just say "yes" or "no" — it tells you which strain you’re carrying. If you’re over 30, many doctors now combine HPV testing with your Pap smear. This combo is more accurate than either test alone. For women under 30, HPV testing isn’t usually done by itself because the virus often clears on its own. But if your Pap result is unclear, they might test for HPV to decide what to do next.
Men don’t routinely get HPV tests, but that doesn’t mean they’re off the hook. HPV can cause cancers of the throat, anus, and penis. While there’s no approved screening test for men, the HPV vaccine, a preventive shot that protects against the most dangerous strains of the virus. Also known as Gardasil, it’s recommended for boys and girls starting at age 11 or 12. Getting vaccinated before exposure is the best way to avoid long-term problems. And if you’ve had an abnormal Pap result, your partner might be advised to get checked too — not for testing, but to understand transmission risks.
What happens after a positive HPV test? It depends. If your Pap is normal and you have a low-risk strain, you might just need to come back in a year. If you have a high-risk strain and abnormal cells, your doctor will likely refer you for a colposcopy — a simple procedure where they look closely at your cervix with a magnifying tool. Sometimes they take a tiny tissue sample to be sure. The good news? Most abnormal results don’t mean cancer. They mean early warning signs — and that’s exactly what HPV testing is for: catching things early when they’re easiest to treat.
You might be wondering if you still need testing after getting the HPV vaccine. Yes — the vaccine doesn’t cover every strain, and it doesn’t help if you were already infected. Testing is still the only way to know if something’s developing. And if you’ve had a hysterectomy? It depends. If your cervix was removed and you had no history of cancer or pre-cancer, you may not need screening anymore. But if your cervix is still there — even after menopause — you still need regular checks.
There’s no magic fix for HPV. No supplements, no teas, no special diets will make it go away. What works is time, monitoring, and medical care. That’s why knowing when to get tested — and what to do next — matters more than ever. Below, you’ll find real stories and practical guides on how HPV testing fits into your health routine, what to ask your doctor, and how to understand your results without panic or confusion.
HPV causes most cervical cancers, but vaccination and modern screening can prevent them. Learn how HPV testing every 5 years, self-collection kits, and vaccines are changing cancer prevention.
READ