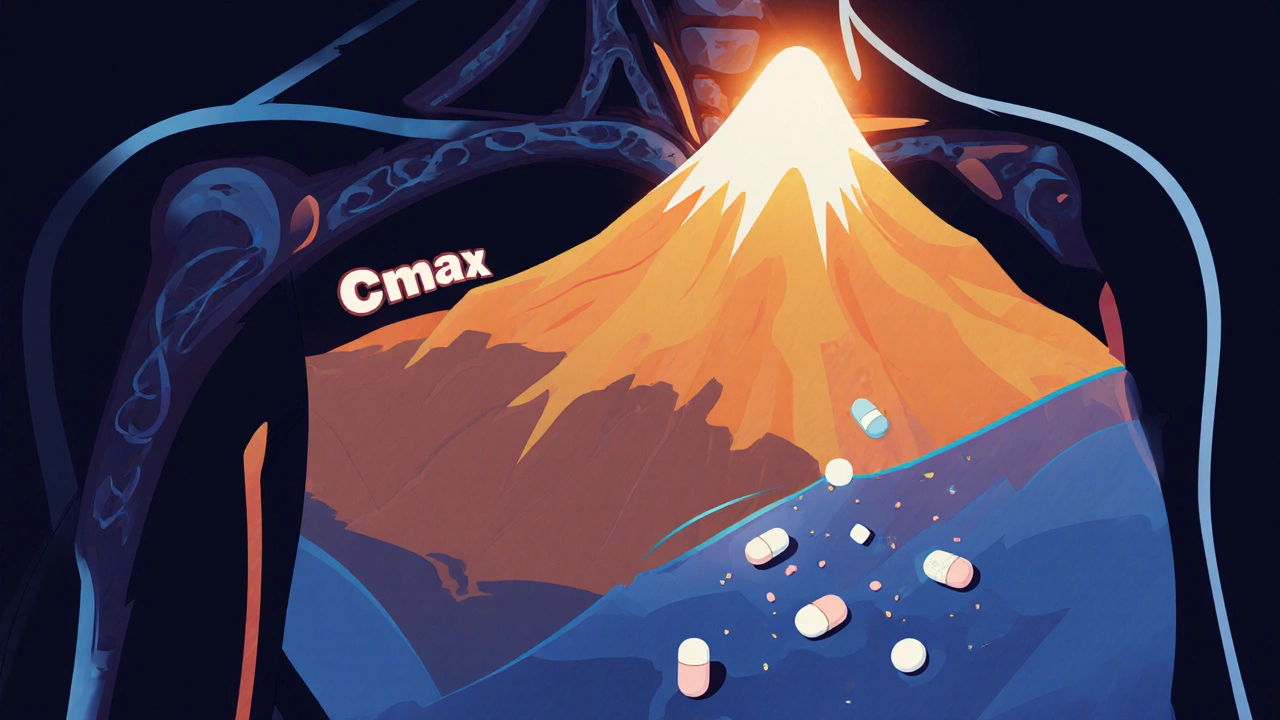
When you take a pill, it doesn’t hit you all at once. It travels through your stomach, gets absorbed into your blood, and eventually reaches its peak concentration, the highest level of a drug in your bloodstream after ingestion. Also known as Cmax, this moment determines when the medicine is most active—and when side effects are most likely to show up. If you don’t know when this happens, you might take your next dose too soon, risk overdose, or miss the window when the drug works best.
Drug absorption, how quickly and completely a medication enters your bloodstream plays a huge role. Some drugs peak in 30 minutes, others take 4 hours. Grapefruit juice can slow absorption of statins. High-fat meals delay the peak of certain antibiotics. Even the time of day you take a pill changes how fast it reaches blood drug levels, the measurable amount of a drug circulating in your plasma. That’s why your doctor asks if you took it with food or on an empty stomach. It’s not just a formality—it’s science.
Medication timing, when you take a drug relative to meals, sleep, or other meds isn’t random. For example, ticagrelor works faster than clopidogrel because it reaches peak concentration quicker, giving heart patients better protection right after a stent. If you miss a dose of a drug that peaks in 2 hours, waiting 6 hours to take it might leave you unprotected during a critical window. On the flip side, doubling up after a missed dose of a drug with a narrow safety margin—like colchicine or warfarin—can land you in the ER.
It’s not just about the drug itself. Your liver, kidneys, age, and even your gut bacteria affect how fast you reach peak concentration. That’s why generic drugs aren’t always interchangeable in practice—even if they’re chemically identical. One person’s peak might hit at 1.5 hours, another’s at 3.5. That’s why post-market studies track real-world results, not just lab numbers. And that’s why knowing your own body’s pattern matters more than any brochure.
Some meds are designed to avoid a sharp peak—extended-release versions spread the dose out to reduce side effects. But if you crush them or open a capsule, you destroy that design and force an unsafe spike in blood levels. Same goes for supplements: St. John’s wort can speed up how fast your body clears a drug, lowering its peak and making it useless. Kava, on the other hand, can slow clearance, pushing levels too high and risking liver damage.
Understanding peak concentration helps you take control. It’s why medication reviews ask when you feel the best—or worst—after taking your pills. It’s why pharmacists check for interactions between antibiotics and painkillers. It’s why you shouldn’t guess when to take your next dose. This isn’t theoretical. It’s daily safety. The posts below show real cases where timing, food, and drug combos made all the difference—whether it’s avoiding deadly toxicity with colchicine, making sure your migraine med hits when you need it most, or knowing why your heart drug needs to be taken on an empty stomach. You’ll find practical tips, comparisons, and warnings from real patients and doctors. No fluff. Just what you need to stay safe and get the most out of your meds.
Cmax and AUC are the two key metrics used to prove that generic drugs work just like brand-name ones. Learn what they measure, why both are required, and how regulators ensure safety and effectiveness.
READ