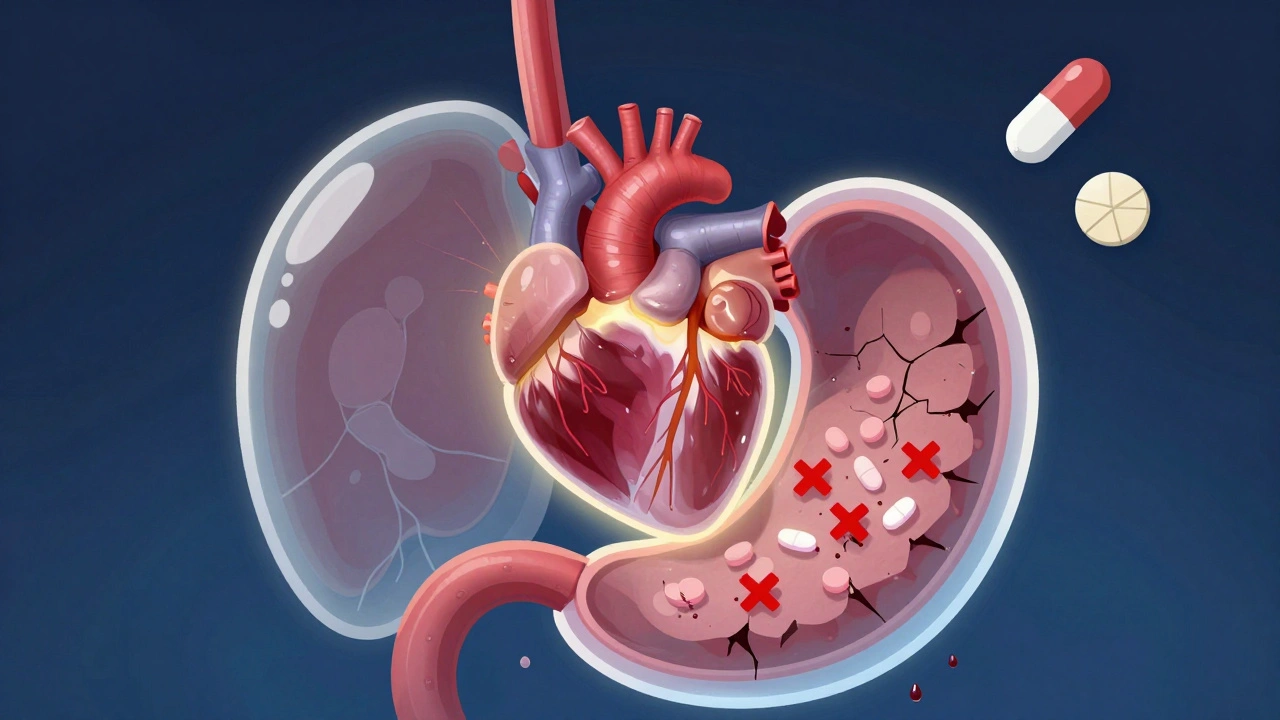
When you take a proton pump inhibitor, a class of drugs used to reduce stomach acid, commonly prescribed for GERD or ulcers along with clopidogrel, an antiplatelet medication used to prevent blood clots after heart attacks or stents, you might think you’re just managing two separate conditions. But science shows this combo can quietly undo the life-saving benefits of clopidogrel. The PPI with clopidogrel interaction isn’t just a theoretical concern—it’s a real, documented risk that’s led to heart attacks in people who followed their doctor’s orders exactly.
Here’s why it happens: clopidogrel needs to be activated by an enzyme in your liver called CYP2C19. Some PPIs, especially omeprazole and esomeprazole, block that same enzyme. That means clopidogrel can’t do its job—your blood stays clot-prone, and your heart stays at risk. Studies from the FDA and major cardiology journals found patients on this combo had up to a 50% higher chance of another heart event. It’s not about taking too much—it’s about taking the wrong mix. Not all PPIs are equal here. Pantoprazole and dexlansoprazole interfere much less, and some doctors now switch patients to those if acid control is still needed.
This isn’t just about pills. It’s about your heart. If you’ve had a stent, a heart attack, or peripheral artery disease, clopidogrel is likely keeping you alive. But if your doctor also gave you a PPI for heartburn, you might be walking around with a hidden flaw in your treatment plan. Many patients don’t even know this interaction exists. They assume all meds work together nicely. But drugs aren’t like vitamins—they’re precision tools, and some combinations cancel each other out. The good news? You have options. You can switch PPIs, use H2 blockers like famotidine instead, or adjust timing. You can also ask about newer antiplatelets like ticagrelor, which don’t rely on that same liver pathway.
What you’ll find below are real, practical guides from people who’ve been there. From how to talk to your doctor about this without sounding alarmist, to what to do if you’ve already been on both meds for months, to alternatives that actually work without risking your heart. These aren’t theory pieces—they’re action plans written by patients and clinicians who’ve seen the fallout of this interaction firsthand. You don’t need to guess. You don’t need to hope. You just need to know what to ask for—and what to avoid.
Antiplatelet medications save lives but raise the risk of dangerous stomach bleeding. Learn how to protect your GI tract with PPIs, avoid NSAIDs, and manage risks without stopping your heart meds.
READ