Heart Medications and Their Dangerous Combinations: What to Avoid
Every year, tens of thousands of people in the U.S. end up in the hospital-or worse-because they took two medications that shouldn’t have been mixed. Many of these cases involve heart drugs, which are often prescribed alongside other pills for pain, sleep, or even supplements people think are harmless. The truth is, some combinations can stop your heart from beating properly, cause internal bleeding, or send your potassium levels soaring to dangerous levels. You don’t need to be a doctor to understand which ones to avoid. You just need to know what’s on your own medicine cabinet.
Why Heart Medications Are Especially Risky
Heart medications don’t just treat symptoms-they change how your body works at a deep level. They control your blood pressure, regulate your heartbeat, thin your blood, or remove extra fluid. When you add another drug on top, it can interfere with those delicate systems. This isn’t rare. In 2022, nearly 57% of women and 44% of men over 65 were taking five or more prescription drugs a week. That’s not just common-it’s the new normal. And with each added pill, your risk of a bad reaction grows.
One major study from the USC Schaeffer Center found that taking just two medications with known cardiovascular side effects doubled the chance of a heart attack, stroke, or death-even in people who had never had heart problems before. Add a third, and that risk jumps by over 200%. These aren’t theoretical risks. They’re happening right now, in living rooms and nursing homes across the country.
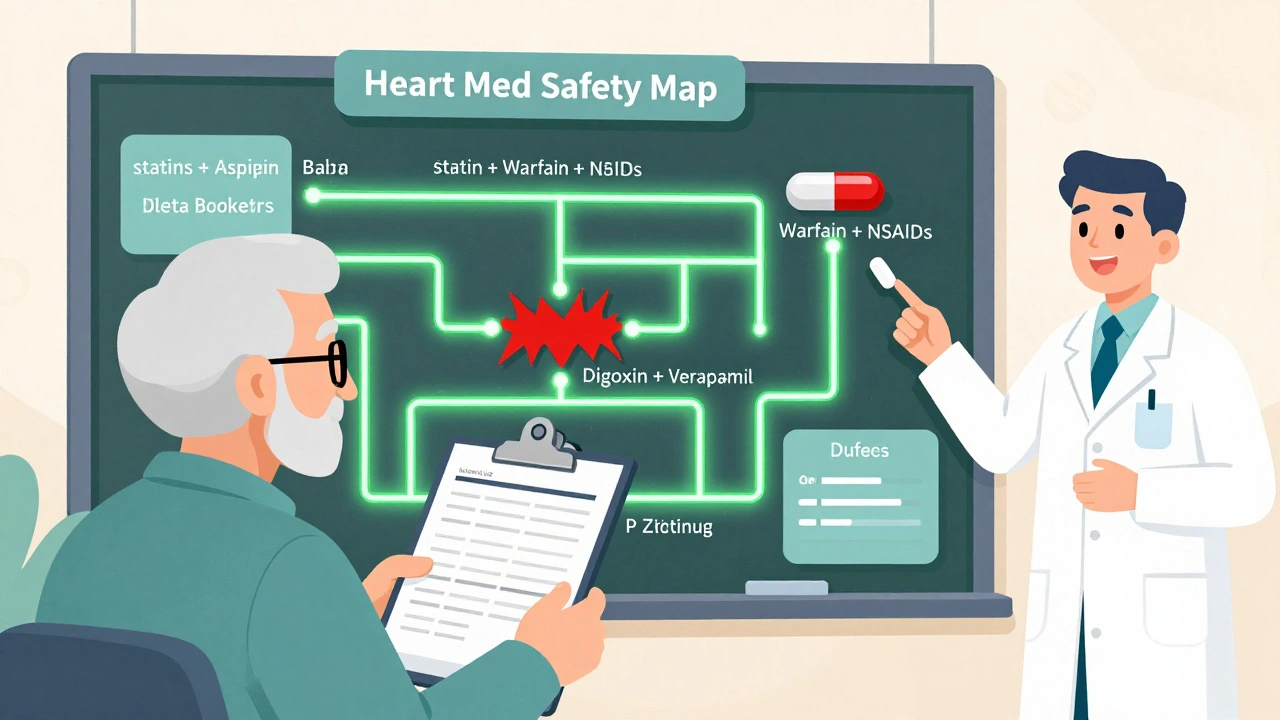
The 7 Most Dangerous Combinations to Avoid
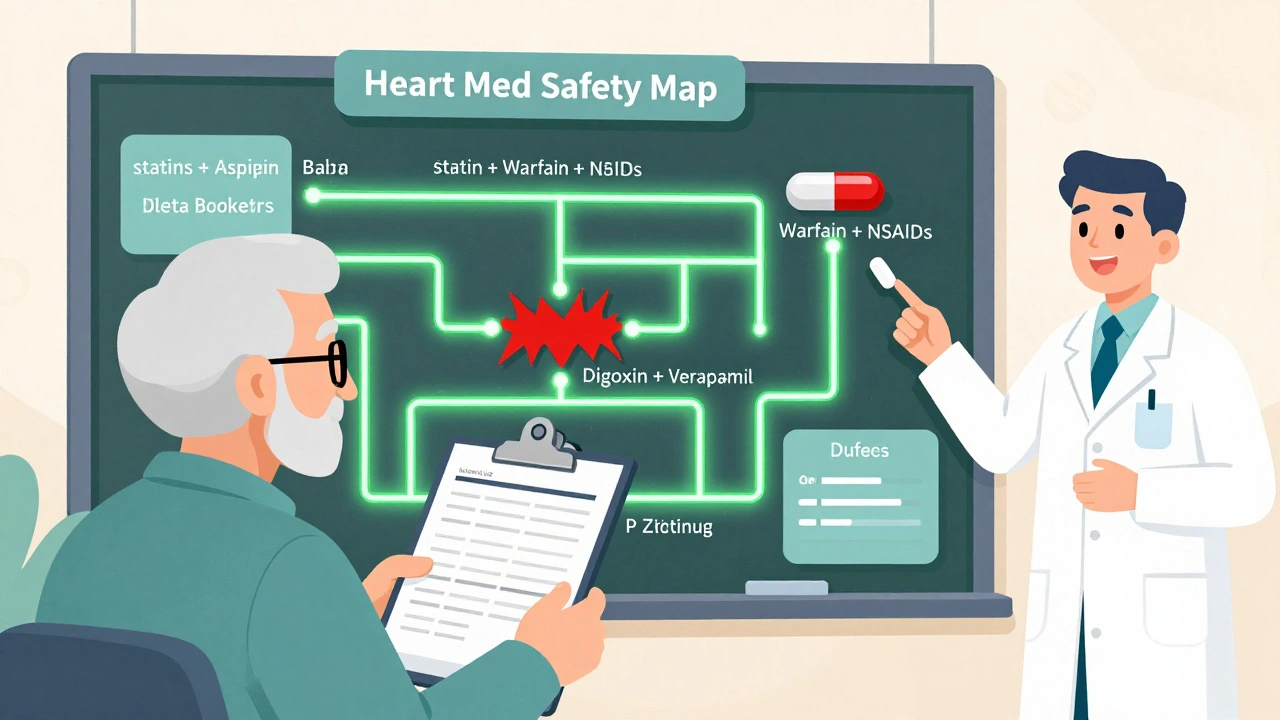
Some drug pairs are so dangerous they come with FDA black box warnings-the strongest safety alert a drug can carry. Here are the top combinations you need to know about.
- Warfarin and ibuprofen: Warfarin thins your blood to prevent clots. Ibuprofen, a common painkiller, irritates your stomach lining and makes it harder for your blood to clot. Together, they can cause serious internal bleeding. Studies show this combo increases GI bleeding risk by 300%. One patient I spoke with ended up in the ER after a dental cleaning because she took ibuprofen for pain the night before. Her INR (a blood clotting measure) was over 8.0-normally it’s between 2 and 3 for someone on warfarin.
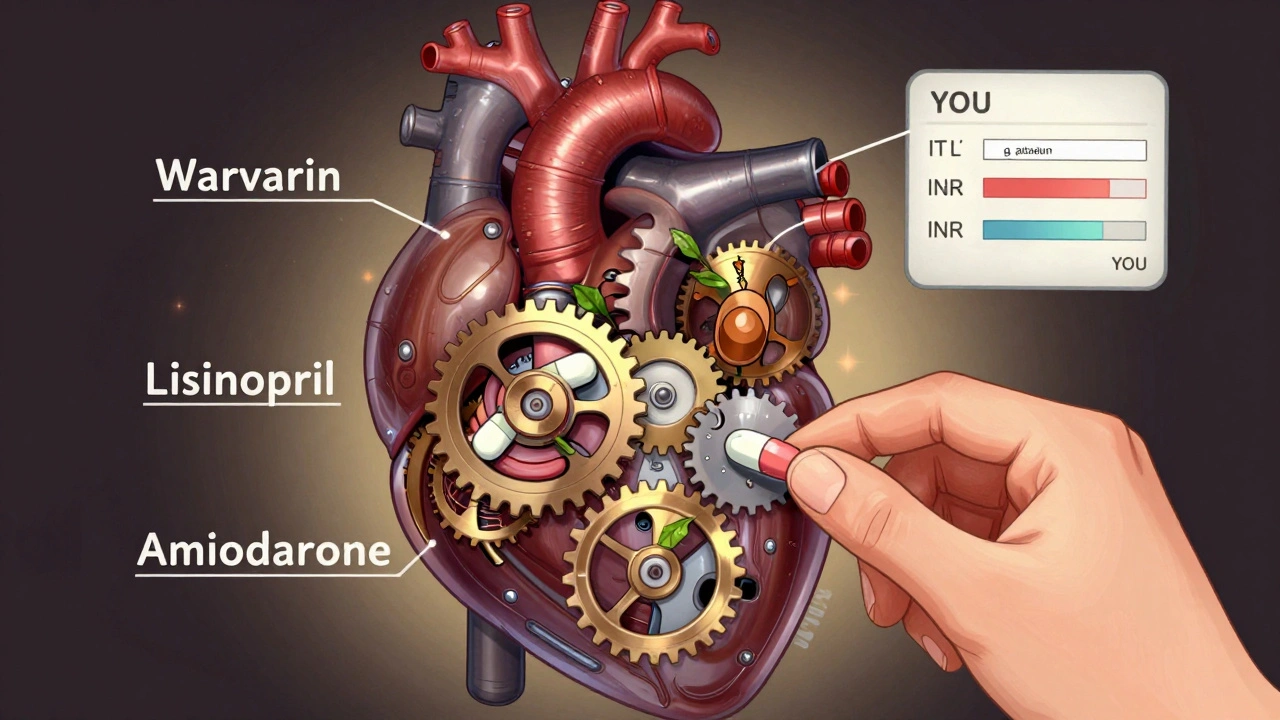
- Warfarin and acetaminophen: Even Tylenol isn’t safe if you’re on warfarin long-term. Chronic use can raise your INR by 2 to 3 points, putting you at risk for spontaneous bleeding. It doesn’t happen right away, which is why many people don’t connect the dots.
- PDE-5 inhibitors (like Viagra) and nitrates: If you’re taking nitroglycerin for chest pain or any other nitrate-based heart medication, never take sildenafil (Viagra), tadalafil (Cialis), or vardenafil (Levitra). Together, they can drop your blood pressure to life-threatening levels-sometimes below 70 mmHg. This combo has caused sudden deaths, even in otherwise healthy men.
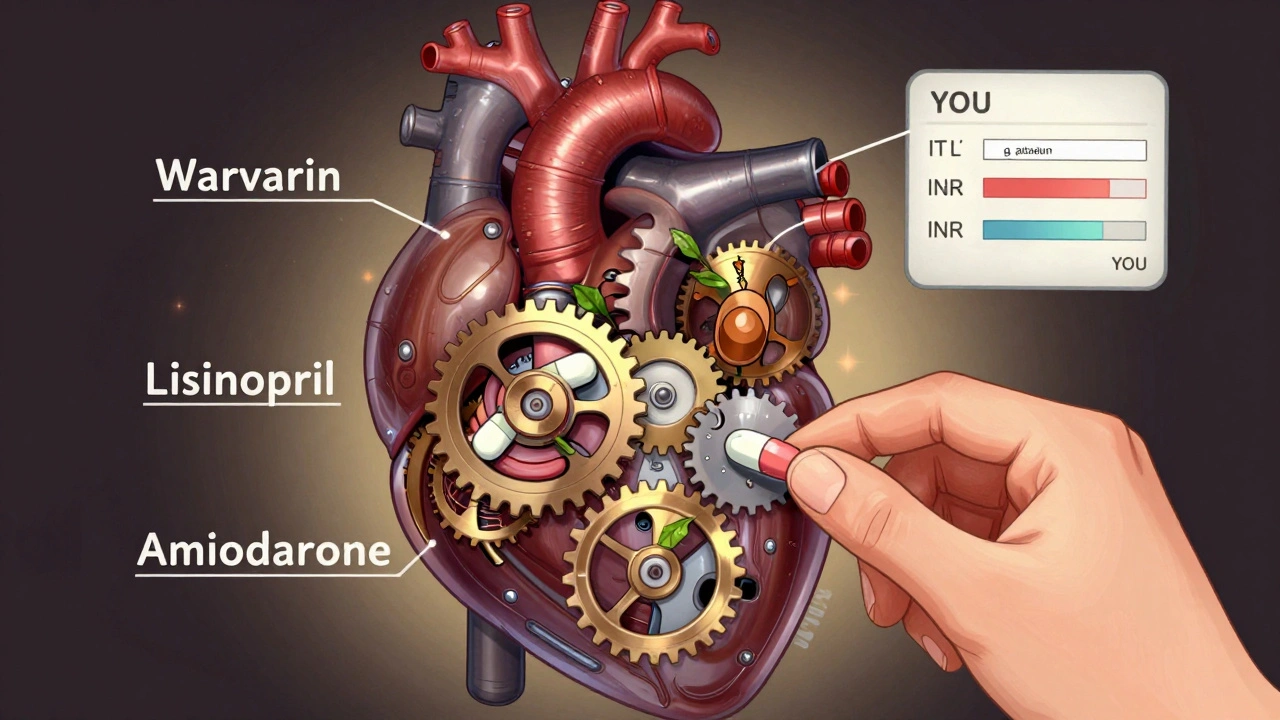
- Statins and amiodarone: Amiodarone is used to treat irregular heartbeats. Statins lower cholesterol. But when taken together, they can cause severe muscle damage (rhabdomyolysis). The risk goes up by 400-500%. Symptoms include intense muscle pain, weakness, and dark urine. If you notice this, stop both drugs and get help immediately.
- ACE inhibitors and potassium supplements: ACE inhibitors like lisinopril or enalapril help relax blood vessels. But they also cause your body to hold onto potassium. Add a potassium pill or salt substitute, and your levels can spike past 5.5 mEq/L. That’s dangerous. High potassium can stop your heart. One 2021 study found 18.7% of patients on this combo had dangerous levels-nearly five times higher than those not taking both.
- Digoxin and verapamil: Digoxin helps control heart rate. Verapamil is a calcium channel blocker used for high blood pressure and arrhythmias. Together, they cause digoxin to build up in your blood by 60-75%. That leads to nausea, confusion, vision changes, and even fatal heart rhythms. This interaction is so well-documented, it’s taught in medical schools.
- NSAIDs and blood pressure meds: Diclofenac, naproxen, and even aspirin (in high doses) can undo the benefits of your blood pressure pills. They cause your body to hold onto fluid, raise your blood pressure, and reduce the effectiveness of diuretics by up to 30%. Over 70 million NSAID prescriptions are written each year in the U.S.-many for people with heart failure. That’s a recipe for hospitalization.
What About Supplements? They’re Not Always Safe
People assume supplements are harmless because they’re sold over the counter. That’s a dangerous myth. St. John’s wort, turmeric, garlic, and ginkgo biloba can all interfere with heart meds.
St. John’s wort speeds up how your liver breaks down warfarin, making it less effective. That means clots can form when you think you’re protected. Turmeric acts like a natural blood thinner and can increase bleeding risk when paired with warfarin or aspirin. Garlic can lower blood pressure too much if you’re already on ACE inhibitors or beta blockers.
A 2021 study in the New England Journal of Medicine found that nearly half of heart patients were taking at least one supplement without telling their doctor. And 62% of those patients said their provider never asked.
What About the “Good” Combinations?
Not all combinations are bad. In fact, some are life-saving. Statins, aspirin, and beta blockers used together have been shown to improve survival by 25-30% in high-risk patients. Newer drugs like SGLT2 inhibitors (dapagliflozin, empagliflozin) are now being combined with standard heart failure treatments-and they reduce hospitalizations by 14%.
Even better, drugmakers are starting to create “polypills”-single pills that combine proven heart medications. AstraZeneca launched one in 2024 that includes dapagliflozin, sacubitril, and valsartan. Early results show better adherence and fewer side effects because patients aren’t juggling five different pills.
How to Protect Yourself
You don’t have to guess which drugs are safe. Here’s what actually works:
- Keep a written list of every pill, patch, vitamin, herb, and OTC drug you take-including doses and why you take them. Update it every 30 days. Write “lisinopril 10 mg daily for blood pressure,” not just “blood pressure pill.”
- Use one pharmacy for all your prescriptions. Pharmacists are trained to catch dangerous interactions. If you switch pharmacies, they lose the full picture.
- Ask your pharmacist every time you get a new script: “Does this interact with anything else I’m taking?” Don’t wait for them to tell you. Ask.
- Review your meds with your doctor at least once a year. Bring your list. Ask: “Is every pill still necessary?” Many older adults take drugs they no longer need.
- Know your numbers. If you’re on warfarin, know your INR. If you have heart failure, know your sodium and potassium levels. Ask for copies of your lab results.
The Beers Criteria, updated in 2023, lists 30 dangerous combinations specifically for people over 65. Your doctor should be familiar with it. If they aren’t, ask for a referral to a geriatric pharmacist or a medication therapy management (MTM) program. Medicare Part D covers these sessions at no cost.
What to Do If You’ve Already Taken a Dangerous Combo
If you’ve taken ibuprofen with warfarin, or NSAIDs with lisinopril, don’t panic-but don’t ignore it either. Watch for:
- Unusual bruising or bleeding (nosebleeds, blood in stool, heavy periods)
- Swelling in your legs or belly
- Extreme fatigue, dizziness, or confusion
- Dark urine or muscle pain
- Irregular heartbeat or chest tightness
If you notice any of these, call your doctor or go to urgent care. Don’t wait. Some reactions take days to show up. Others happen within hours.
Why Doctors Miss These Risks
A 2023 report found that only 37% of primary care doctors routinely screen for dangerous drug combinations during visits. Why? Time. Too many patients. Too many pills. Too little training on interactions.
But the system is changing. The FDA now requires updated warnings on 27 heart medications. Medicare penalizes hospitals for readmissions due to medication errors. AI tools are being rolled out to flag risky combos in real time. Still, the biggest gap remains: patients aren’t speaking up.
Final Thought: Your Meds Are Not a Puzzle to Solve Alone
Heart medications save lives-but only if they’re used right. The danger isn’t in taking one drug. It’s in taking the wrong mix. You don’t need to memorize every interaction. You just need to be the one asking the questions. Bring your list. Ask about every new pill. Tell your pharmacist about the turmeric you take for arthritis. Say no to over-the-counter painkillers unless your doctor says yes.
Your heart doesn’t care if the pill came from a pharmacy or a health food store. It only cares if it’s safe to take with the rest. Don’t let silence be your risk factor.
Can I take ibuprofen if I’m on a blood thinner like warfarin?
No. Ibuprofen and other NSAIDs significantly increase your risk of dangerous internal bleeding when taken with warfarin. Even occasional use can raise your INR and lead to hospitalization. Use acetaminophen (Tylenol) instead, but only if your doctor approves it and you don’t take it long-term. Always check with your pharmacist before taking any pain reliever.
Is it safe to take St. John’s wort with heart medications?
No. St. John’s wort speeds up how your body breaks down warfarin, digoxin, and some beta blockers, making them less effective. This can lead to blood clots, irregular heartbeats, or worsening heart failure. Many people take it for depression without realizing it interferes with their heart drugs. Always tell your doctor about every supplement you use.
Can I take potassium supplements if I’m on an ACE inhibitor?
Not without close monitoring. ACE inhibitors like lisinopril already cause your body to retain potassium. Adding a potassium supplement can push your levels above 5.5 mEq/L, which can cause your heart to stop suddenly. This combination is responsible for nearly one in five cases of dangerous hyperkalemia in older adults. Only take potassium if your doctor orders it and checks your blood levels regularly.
What should I do if I accidentally take a dangerous combination?
Stop taking both medications immediately. Call your doctor or go to urgent care. If you have symptoms like unusual bleeding, chest pain, confusion, swelling, or dark urine, go to the ER. Don’t wait. Some reactions are slow, but others can be life-threatening within hours. Bring your medication list with you.
Are there any heart medication combos that are actually good?
Yes. Combining statins, aspirin, and beta blockers has been shown to improve survival by 25-30% in high-risk patients. Newer drugs like SGLT2 inhibitors (dapagliflozin) also work well with standard heart failure treatments, reducing hospitalizations by 14%. Some drugmakers are now combining these into single pills called “polypills,” which improve adherence and reduce side effects.
How can I make sure my doctor knows all my medications?
Bring a written, up-to-date list to every appointment-including prescriptions, over-the-counter drugs, vitamins, herbs, and supplements. Include the dose and how often you take it. Use one pharmacy for all your prescriptions so your pharmacist has a full record. Ask your doctor: “Is every pill I’m taking still necessary?” Many people take medications they no longer need.
Can I use a pill organizer to avoid mistakes?
Pill organizers help with timing, but they don’t prevent dangerous interactions. If you’re taking a harmful combo, putting both pills in the same compartment doesn’t make it safer. The key is knowing which drugs shouldn’t be taken together. Use the organizer as a tool, not a solution. Always talk to your pharmacist or doctor before adding any new pill-even if it’s in your organizer.
Next Steps: What You Can Do Today
1.
Write down every medication you take-including doses and reasons. Include supplements and OTC drugs. Do it now, before your next appointment.
2.
Call your pharmacy and ask them to review your list for dangerous interactions. They’re trained to do this, and it’s free.
3.
Ask your doctor if any of your meds can be stopped. Many older adults take unnecessary pills.
4.
Never take a new OTC drug without checking with your pharmacist first.
Your heart doesn’t need more pills. It needs the right ones-and no dangerous combinations.
12 Responses
I took ibuprofen with warfarin once after a toothache. Didn't think anything of it. Ended up in the ER with a nosebleed that wouldn't stop. Don't be me.
I'm so glad someone finally said this. My mom was on like 8 meds and no one ever checked for interactions. She had a near-miss with potassium overload because her doctor didn't know she was taking salt substitute. We're switching to a geriatric pharmacist now. Thank you for the list.
This is the kind of post that makes me believe in the power of shared knowledge. So many of us are just trying to survive our own health systems. You didn't just list dangers-you gave us tools. That’s rare. Thank you.
Oh please. Another fear-mongering article from someone who thinks every pill is a death sentence. People have been mixing ibuprofen and warfarin for decades. I’ve known three people who did it and they’re all fine. The real danger is letting Big Pharma scare you into thinking you need a PhD to take a pill. Wake up.
You think this is bad? Try living in a country where the government gives you a pill for sneezing. We’re turning into a nation of hypochondriacs who think their liver needs a babysitter. The FDA doesn’t know what it’s doing. Half these warnings exist because lawyers made more money than doctors.
I’ve spent over two decades in the pharmaceutical industry, and I can tell you this: the data behind these interactions is not just robust-it’s overwhelming. The problem isn’t the science. The problem is the system. Doctors are overworked, pharmacists are understaffed, and patients are told to ‘just take it’ without context. This isn’t paranoia. It’s epidemiology. And if you’re not paying attention, you’re not just risking your health-you’re risking your family’s peace of mind.
I’m from South Africa. We don’t have the same access to meds here. But I’ve seen people die because they took aspirin with blood pressure pills because they thought ‘natural’ meant ‘safe.’ Your post? It’s not just for Americans. It’s for everyone who’s ever been told ‘it’s just a supplement.’
I’m so proud of you for writing this. 💪 I’ve been on 5 heart meds since 55 and I finally started using a pharmacy that does med reviews. My INR stabilized within a week. You’re not just saving lives-you’re giving people back their peace. Thank you.
I must respectfully assert that the assumption that over-the-counter supplements are inherently benign is a dangerous fallacy predicated upon cultural naivete and a systemic failure of public health education. The regulatory vacuum surrounding herbal products creates an environment wherein pharmacological autonomy is not only compromised but actively weaponized by marketing narratives that exploit consumer trust. The solution lies not in fear but in institutional accountability
As a physician from India, I can confirm these interactions are equally prevalent in our healthcare system. Many patients bring herbal remedies from home without disclosure. We have started mandatory medication reconciliation forms in our clinics. Your point about using one pharmacy is critical. We need more awareness, not more pills.
I read this whole thing and then Googled ‘is turmeric bad with blood thinners’ and yes it is. Also I just took one because my knee hurt. Oh god. I’m gonna die. I’m gonna die and it’s gonna be because I thought ‘it’s just a spice’ and now my blood is liquid. Someone call my mom.
I used to think my grandma was being dramatic when she’d say ‘I don’t trust these pills’-until I saw her face when she found out her garlic supplement was messing with her BP meds. She cried. Not because she was scared-but because she felt stupid. You don’t need to be a genius to get this right. You just need someone to care enough to ask. And now? I ask. Every. Single. Time.