When you take an antibiotic, a medicine designed to kill or slow the growth of bacteria. Also known as antibacterial agents, these drugs only work if your body can pull them into your bloodstream effectively. That process is called antibiotic absorption, how the drug moves from your digestive system into your blood. It doesn’t matter how strong the antibiotic is—if it doesn’t get absorbed, it won’t help. This isn’t just science talk. It’s the difference between getting better and staying sick.
Not all antibiotics absorb the same way. Some work best on an empty stomach, like antibiotic absorption for amoxicillin or ciprofloxacin, because food can block them. Others, like doxycycline, shouldn’t be taken with dairy—calcium binds to the drug and stops it from entering your system. Even antacids, iron pills, or calcium supplements can interfere. You might think you’re doing everything right by taking your pill with water, but if you’re also taking a multivitamin or heartburn medicine, you could be neutralizing your treatment. This is why timing matters as much as the dose.
Bioavailability, the percentage of the drug that actually enters circulation. is the technical term for how much of your antibiotic gets used. A drug with 90% bioavailability means almost all of it works. One with 30%? You’re wasting most of it. That’s why doctors pick certain antibiotics for certain infections—it’s not just about what kills the bug, but what your body can actually use. Even your gut health plays a role. If you’ve been on antibiotics before, or have digestive issues like Crohn’s or celiac disease, your absorption might be lower. That’s not something most people realize until they’re not getting better.
And then there’s the flip side: what happens when absorption is too good? Some antibiotics build up too quickly, causing side effects like nausea, dizziness, or even kidney stress. That’s why extended-release versions exist—they spread out absorption to avoid spikes. It’s not just about getting the drug in. It’s about getting it in at the right speed.
You don’t need a pharmacy degree to make this work. But you do need to know the basics: when to take it, what to avoid, and how to spot if it’s not working. The posts below break down real cases—like why someone’s doxycycline failed because they took it with yogurt, or how a patient’s ciprofloxacin didn’t help because they were also on an antacid. You’ll find guides on how to time your doses around meals, what supplements to pause, and why some antibiotics work better with certain foods. There’s even a post on how drug interactions can block absorption without you even knowing it. These aren’t theory pages. These are fixes for people who took their medicine and still felt worse.
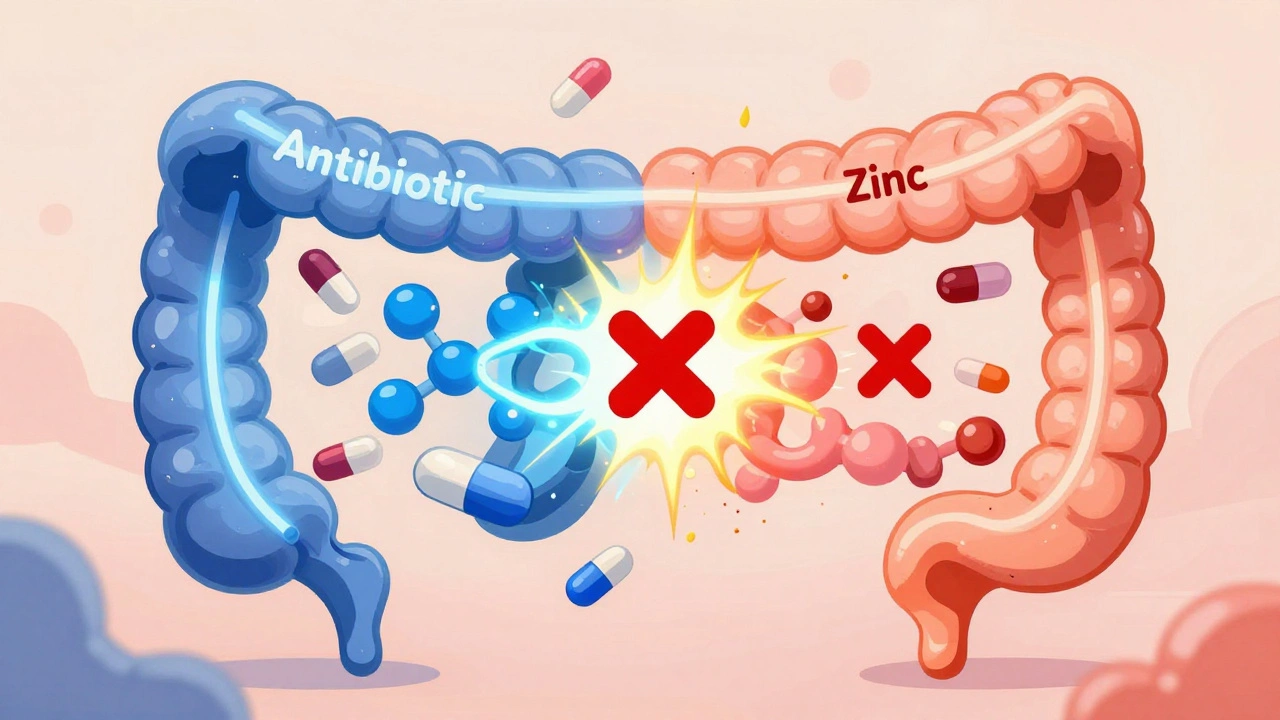
Zinc supplements can block the absorption of key antibiotics like doxycycline and ciprofloxacin. Learn how to time doses properly-2 to 6 hours apart-to ensure your treatment works and avoid treatment failure or antibiotic resistance.
READ