When it comes to HPV prevention, the process of reducing infection risk from human papillomavirus, a common virus linked to several cancers. Also known as human papillomavirus prevention, it’s one of the few cancer-prevention strategies you can act on today. HPV isn’t just a concern for women—it affects everyone, regardless of gender or sexual activity. Nearly 80% of sexually active people will get at least one type of HPV in their lifetime. Most clear on their own, but some strains stick around and can lead to cervical, throat, anal, or penile cancers. That’s why prevention isn’t optional—it’s essential.
The most powerful tool in HPV prevention, the strategy to stop infection before it starts is the HPV vaccine, a safe, two- or three-dose shot that protects against the cancer-causing strains of the virus. It works best when given before exposure, which is why it’s recommended for kids as young as 9, but adults up to age 45 can still benefit. The vaccine doesn’t treat existing infections, but it stops new ones. It’s not just for teens—it’s for anyone who hasn’t been fully vaccinated yet. Pair that with regular screenings like Pap tests and HPV DNA tests, and you’re covering both prevention and early detection.
Cervical cancer, a preventable disease caused by persistent high-risk HPV infection used to be a leading cause of death in women. Thanks to screening and vaccination, rates have dropped sharply. But progress isn’t universal. Many people still skip the vaccine because they think it’s only for teens, or they don’t realize HPV causes more than just cervical cancer. Others delay Pap tests because they feel fine—yet HPV often shows no symptoms until damage is done. Prevention isn’t about fear. It’s about control. You can’t always stop exposure, but you can stop the outcome.
Condoms help reduce transmission, but they don’t block all skin-to-skin contact where HPV lives. That’s why relying on them alone isn’t enough. The real game-changer is combining vaccination with routine medical checkups. Even if you’ve had HPV before, the vaccine can still protect you from other strains. And if you’re over 26, talk to your doctor—new guidelines are expanding eligibility. This isn’t just a women’s health issue. Men can carry and spread HPV, and they’re at risk for throat and anal cancers too. Prevention works best when everyone participates.
Below, you’ll find real-world advice on how to talk to your doctor about HPV, what the vaccine actually covers, how to spot signs you might have missed, and why skipping screenings puts you at risk—even if you feel fine. These aren’t theoretical tips. They’re based on what people actually need to know to stay safe.
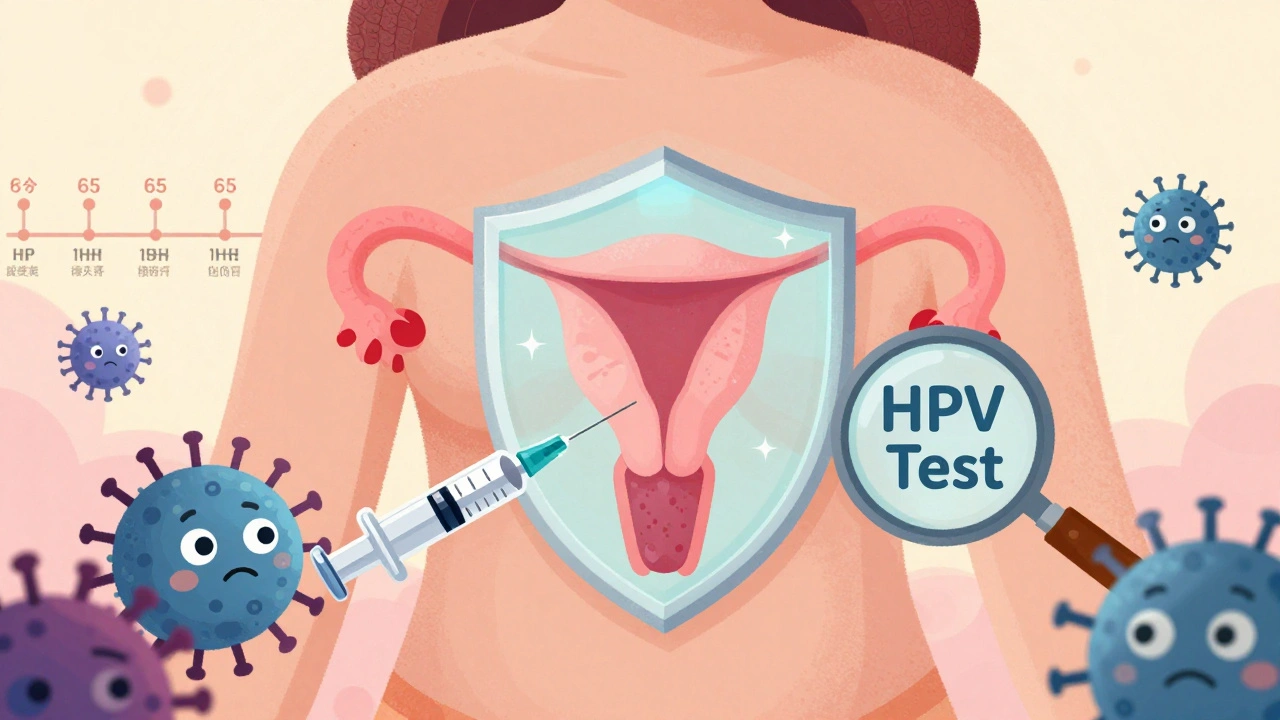
HPV causes most cervical cancers, but vaccination and modern screening can prevent them. Learn how HPV testing every 5 years, self-collection kits, and vaccines are changing cancer prevention.
READ