When you take a pill, injection, or cream, systemic exposure, the total amount of a drug that reaches your bloodstream and circulates throughout your body. Also known as total drug exposure, it determines how strongly and for how long a medication works—or causes side effects. It’s not just about how much you swallow or apply. Two people taking the same dose can have wildly different systemic exposure because of age, liver function, other drugs, or even what they ate that day.
This is why drug interactions, when one substance changes how another is absorbed, broken down, or cleared. Also known as pharmacokinetic interactions, it can turn a safe dose into a dangerous one. Take colchicine and clarithromycin together? That combo blocks the body’s ability to clear colchicine, spiking systemic exposure and risking life-threatening toxicity. Same with grapefruit juice and statins—it slows down liver enzymes that normally break down the drug, letting too much build up in your blood. Even something as simple as skipping a meal can change how fast a drug gets absorbed, altering systemic exposure.
pharmacokinetics, how your body moves a drug through absorption, distribution, metabolism, and elimination. Also known as ADME, it is the science behind systemic exposure. It’s why some drugs need to be taken on an empty stomach, why some are dosed once a day and others four times, and why older adults often need lower doses. Your liver and kidneys are the main filters—if they’re not working well, systemic exposure climbs, even if you take the same amount. That’s why medication reviews are so important: they check if your current drugs are still safe given your body’s changing ability to handle them.
Systemic exposure isn’t just about danger—it’s also about effectiveness. Too little, and the drug won’t work. Too much, and you risk side effects or overdose. That’s why post-market studies track real-world use: to catch cases where systemic exposure goes off the rails because of genetic differences, new drug combinations, or poor adherence. Generic drugs aren’t less safe—they’re just monitored more closely after launch because their systemic exposure must match the brand name exactly to be approved.
When you’re managing chronic conditions like heart disease, migraines, or skin disorders, knowing how your body handles each medication helps you avoid surprises. Ticagrelor works faster than clopidogrel because it reaches systemic exposure quicker. Hydroquinone creams need careful dosing because too much gets absorbed through the skin and can cause long-term damage. Even something like kava, a natural supplement, can raise systemic exposure of sedatives and cause dangerous drowsiness or liver injury.
What you’ll find here isn’t theory—it’s practical, real-world guidance. From how to handle missed doses without doubling up, to why certain antibiotics shouldn’t mix with painkillers, to how to safely dispose of old meds to prevent accidental exposure, every article ties back to one thing: understanding how your body processes what you take. Whether you’re on a single drug or managing multiple prescriptions, knowing about systemic exposure helps you stay in control—not just of your health, but of your treatment.
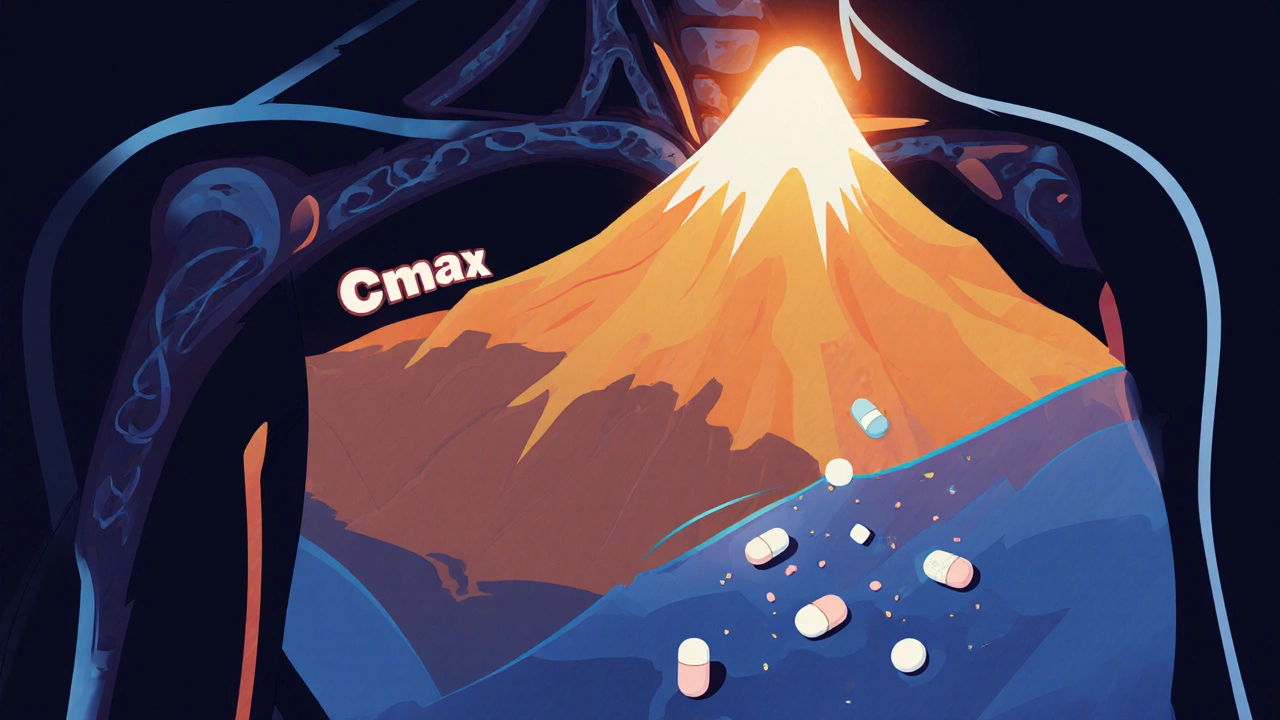
Cmax and AUC are the two key metrics used to prove that generic drugs work just like brand-name ones. Learn what they measure, why both are required, and how regulators ensure safety and effectiveness.
READ