For people stuck in a cycle of 15 or more headache days a month, where migraines blur into a constant storm of pain, nausea, and light sensitivity, finding relief can feel impossible. Many have tried pills-beta-blockers, antidepressants, anti-seizure meds-only to quit because of dizziness, weight gain, brain fog, or worse. That’s where Botox comes in. Not as a quick fix, not for every migraine sufferer, but as a proven, FDA-approved option for those with chronic migraine who’ve run out of other choices.
Botox, or onabotulinumtoxinA, is the same substance used to smooth forehead wrinkles. But when it comes to migraines, it’s working far deeper than just relaxing muscles. It’s interrupting the pain signals at their source.
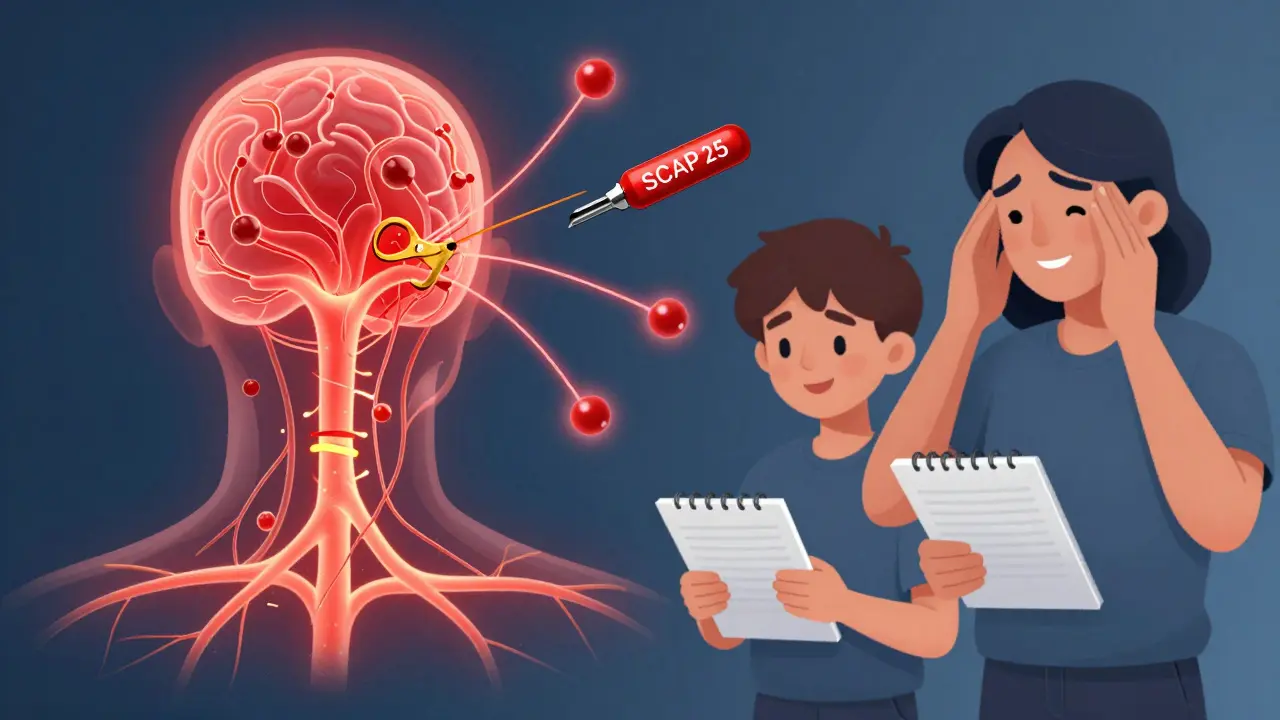
Here’s how: Botox blocks the release of certain chemicals, especially calcitonin gene-related peptide (CGRP), which spikes during a migraine attack and causes inflammation and nerve sensitization. It does this by cutting a protein called SNAP-25, which nerve cells need to send out pain signals. This happens in the trigeminal nerve system-the main pain pathway for headaches. It also reduces inflammation around nerves and dampens the brain’s overall sensitivity to pain over time.
Unlike triptans or gepants that stop an attack once it starts, Botox doesn’t treat acute pain. It’s a preventive tool. Think of it like turning down the volume on your body’s pain alarm system so it doesn’t go off as easily.
Not everyone with headaches qualifies. Botox is only approved for chronic migraine, defined as having headaches on 15 or more days per month, with at least eight of those days meeting migraine criteria-throbbing pain, nausea, sensitivity to light or sound.
If you have fewer than 15 headache days a month, Botox won’t help. Studies show it has no significant effect on episodic migraine. That’s a key point. Many people assume it’s a universal migraine cure. It’s not.
The best candidates are those who’ve tried and failed at least three other preventive medications-like topiramate, propranolol, or amitriptyline-and still can’t get control. It’s also a strong option for people who can’t tolerate oral meds due to side effects, or who have conditions like depression, kidney issues, or pregnancy that limit their choices.
People with medication-overuse headache (a common problem in chronic migraine, affecting nearly half of patients) often see big improvements. So do those with overlapping tension-type headaches or neck stiffness. The more frequent and disabling the headaches, the more likely Botox will make a noticeable difference.
The treatment follows a strict, science-backed protocol called PREEMPT. It’s not random injections. A trained neurologist or headache specialist gives 31 to 39 tiny shots across seven specific areas: forehead, temples, back of the head, neck, and upper shoulders. Each session takes about 15 minutes. The total dose is usually 155 to 195 units.
These aren’t deep muscle injections-they’re placed precisely where pain signals originate. The goal isn’t to paralyze muscles but to block the nerve signals that trigger migraines. You won’t look frozen. Most people don’t notice any change in their facial expressions.
It’s done every 12 weeks. No daily pills. No refills. Just a short office visit, four times a year.
Patience is required. Most people don’t feel the full benefit after the first round. About 61% of patients report their best results after the third or fourth treatment cycle. That means you might need almost a year to know if it’s working for you.
In clinical trials, people saw an average drop of 8 to 9 headache days per month after 56 weeks. Real-world data from over 1,200 patients showed an even bigger drop-12.3 fewer headache days per month after a year. For someone going from 25 headache days to 13, that’s life-changing.
It’s not magic. Some people see only a 20% improvement. Others go from daily pain to just a few days a month. But the biggest win for many isn’t just fewer headaches-it’s fewer rescue meds. People report needing fewer triptans, less painkillers, and less time spent in bed.

Compared to oral preventives, Botox is gentle. The most common side effects are mild: neck pain (about 10% of users), headache right after the shot (7%), and occasional eyelid drooping (3%). That last one is rare and usually temporary.
Less than 1% report muscle weakness in the neck or shoulders that affects daily tasks like holding up your head. That’s why proper technique matters so much. Studies show injector experience accounts for nearly a quarter of treatment success. A poorly placed shot can lead to discomfort or temporary weakness. That’s why you need a specialist trained in the PREEMPT protocol-not just any dermatologist or aesthetic provider.
There’s no risk of addiction. No liver damage. No weight gain. No brain fog. That’s why so many patients switch from pills to Botox-they finally feel like themselves again.
Let’s break it down:
| Treatment | 50% Responder Rate | Common Side Effects | Dosing Frequency | Cost (Annual, Pre-Insurance) |
|---|---|---|---|---|
| Botox (onabotulinumtoxinA) | 47% | Neck pain, headache, eyelid droop | Every 12 weeks | $6,000-$7,200 |
| Topiramate | 39% | Brain fog, tingling, weight loss, kidney stones | Daily | $200-$500 |
| Propranolol | 35% | Fatigue, low blood pressure, dizziness | Daily | $100-$300 |
| Erenumab (CGRP antibody) | 52% | Constipation, injection site reaction | Monthly injection | $8,000-$10,000 |
Botox isn’t the cheapest. But it’s often cheaper than monthly CGRP antibodies and far less disruptive than daily pills with side effects that make life harder. And unlike CGRP drugs, Botox doesn’t require blood tests or long-term safety monitoring.
Some patients even combine Botox with CGRP antibodies. A 2023 study showed that pairing them boosted response rates to nearly 70%. That’s a game-changer for stubborn cases.
Yes, it’s expensive. Without insurance, each session costs $1,500 to $1,800. That’s $6,000 to $7,200 a year.
But here’s the good news: 85% of major U.S. insurers cover it for chronic migraine-if you meet their criteria. That usually means:
Insurance companies often require prior authorization. That means your doctor has to submit records showing you’ve tried other options. This can take weeks. Some patients give up here. But persistence pays off. Many who get denied once get approved after appealing.
There’s also a patient assistance program from the manufacturer that can cut costs significantly for those without coverage.
On forums like Migraine.com and Reddit, people are honest. One user wrote: “After three rounds, I went from 25 migraine days a month to 8-10. My worst ones are now just bad, not debilitating.” Another said: “I stopped taking 12 pills a week. I can finally work full-time.”
But not everyone wins. Some report inconsistent results between cycles. Others say the injections hurt more than expected. And yes, insurance battles are real. One Reddit user spent six months fighting for coverage before finally getting approved.
Still, 58% of users on Migraine.com rated Botox as “significant improvement.” The top reasons? Fewer meds, better sleep, less anxiety about the next attack.
Since its FDA approval in 2010, over a million people have used Botox for migraines. No new safety risks have emerged. There’s no evidence of nerve damage, organ toxicity, or long-term muscle weakness.
The FDA even expanded approval in 2023 to include teens aged 12-17 with chronic migraine. That’s a big deal-it shows confidence in its safety profile.
Studies tracking patients for two years show a 78% retention rate. That means nearly 8 out of 10 people keep using it because it works. If you’re looking for a treatment that’s been tested, trusted, and repeated for over a decade, Botox is one of the few with that track record.
Researchers are working on longer-lasting versions. Early trials suggest a new formulation could last 16 to 20 weeks instead of 12. That means fewer visits, lower cost, and better adherence.
There’s also growing interest in personalizing treatment. Not everyone’s migraine pain comes from the same nerves. Future versions might target specific areas based on where your pain starts-forehead, neck, temples-making it even more effective.
For now, Botox remains a cornerstone of chronic migraine care. It’s not the first thing you try. But for those who’ve tried everything else and still suffer, it’s often the turning point.
If you’re tired of pills that make you feel worse than your headaches, and you’re stuck in the chronic migraine trap, talk to a headache specialist. Bring your headache diary. Ask about Botox. It might not be the answer for everyone-but for the right person, it’s the one thing that finally brings back control.
Yes, it’s the same substance-onabotulinumtoxinA. But the dosage, injection sites, and purpose are completely different. Cosmetic Botox uses fewer units and targets facial muscles to reduce wrinkles. Migraine treatment uses higher doses and targets nerves around the head and neck to block pain signals. It’s administered by neurologists trained in the PREEMPT protocol, not aesthetic providers.
No. Botox is not an acute treatment. It doesn’t work like a triptan or a gepant. It’s designed to prevent migraines over time by reducing nerve sensitivity. If you’re having an attack, you still need your rescue meds. Botox lowers your overall risk of attacks, but it won’t stop one in progress.
Most people don’t see full results until their third or fourth treatment cycle, which takes about a year. Some notice small improvements after the first or second round, but the biggest drops in headache days usually happen after 6 to 9 months. Patience is key. It’s not an instant fix-it’s a long-term strategy.
Not necessarily. Many people continue using acute meds like triptans or NSAIDs while on Botox. In fact, a common goal is to reduce how often you need them. Your doctor may ask you to stop one or two preventive meds to better assess Botox’s effect, but you won’t be told to quit all your medications cold turkey.
Yes. Since its FDA approval for migraines in 2010, over a million patients have used it long-term with no new safety concerns. Studies show no damage to nerves, muscles, or organs. The American Headache Society and European Headache Federation both consider it a safe, first-line option for chronic migraine. The most common side effects are mild and temporary.
Yes. In June 2023, the FDA expanded approval to include adolescents aged 12 to 17 with chronic migraine. This was based on a clinical trial showing an average reduction of 7.8 headache days per month compared to placebo. It’s now a recognized option for teens who haven’t responded to other preventives and need a non-pill alternative.
Your migraine frequency will likely return to pre-treatment levels over several months. Botox doesn’t cure migraine-it manages it. Stopping the injections removes the preventive effect. There’s no rebound effect or worsening of symptoms, but you’ll lose the protection it provided. Most patients who benefit choose to continue indefinitely.
11 Responses
Been on Botox for 2 years now. Went from 22 headache days to 6. No brain fog, no weight gain, just... quiet. Still take sumatriptan when I need it, but I can actually plan stuff now. Life’s weird like that.
Same drug, different purpose. Stop acting like it’s magic.
Let’s clarify the pharmacodynamics: Botox cleaves SNAP-25, inhibiting vesicular release of CGRP and other nociceptive neurotransmitters from peripheral terminals of the trigeminal sensory system. This downregulates central sensitization via reduced glutamatergic input to the trigeminocervical complex. It’s not muscle relaxation-it’s neuromodulation at the synaptic level. The PREEMPT protocol targets specific nociceptive hotspots, not aesthetic zones. Cosmetic dosing is 5–20 units; migraine requires 155–195. Don’t conflate the two.
Why are we giving people shots instead of telling them to just deal with it? This country’s gone soft. Back in my day, we took aspirin and walked it off. Now we need 39 injections and a PhD to understand why our head hurts.
Y’all this changed my LIFE 😭 I went from crying in the bathroom at work every other day to actually attending my kid’s soccer games 🥹 I know it’s not perfect and insurance is a nightmare but if you’re on the fence-just talk to a headache specialist. You deserve to feel human again 💪✨
So Botox is basically the anti-pill? No brain fog, no weight gain, just... chill. I’m low-key jealous of people who get this. Meanwhile I’m still on topiramate and forgetting where I put my keys.
I’ve seen people get discouraged because they don’t see results after one round. But the data shows it takes 3–4 cycles. That’s not failure-that’s biology. If you’ve tried everything else, give it time. It’s not a sprint.
They say 85% of insurers cover it. That’s a lie. My doc submitted 3 times. Got denied every time. Said I didn’t ‘fail’ enough meds. I’ve been on 5. Five. And they still said no. This system is rigged.
America spends billions on this while people can’t afford insulin. We treat pain like a luxury. Botox for migraines? Cool. But why is it so expensive? Because profit > people. 🤷♀️
In India, we don’t have this option easily... but I know someone who went to Bangkok for treatment. It cost less than insurance co-pay here. The irony is, the same drug, same science, but access? Totally different world. 🌍
It’s like someone turned down the volume on your brain’s emergency alarm. You don’t notice the silence until you realize you haven’t flinched at sunlight in weeks. That’s the quiet victory. Not the injections. Not the cost. Just... peace.