
When someone says "type 1 diabetes," most people think of insulin shots and blood sugar checks. But that’s only the surface. Underneath, it’s an autoimmune war inside your pancreas - your own immune system attacking the very cells that make insulin. This isn’t a lifestyle issue. It’s not caused by eating too much sugar. It’s not something you can out-exercise or out-diet. It’s a broken immune response that destroys insulin-producing beta cells, leaving you with almost zero ability to regulate blood sugar on your own.
At diagnosis, most people with type 1 diabetes are producing less than 5% of the insulin their body needs. Their C-peptide levels - the marker that shows your pancreas is still making insulin - are often below 0.2 nmol/L. Compare that to someone with type 2 diabetes, who usually still makes over 0.6 nmol/L. That’s why insulin isn’t optional. It’s life support.
The pancreas has two jobs: making digestive enzymes (exocrine) and making insulin (endocrine). Type 1 diabetes targets only the endocrine part - the islets of Langerhans where beta cells live. The immune system mistakes these cells as invaders. T-cells swarm in, a process called insulitis, and start destroying them. They don’t attack randomly. They go after specific proteins on the beta cells: insulin itself, GAD65, IA-2, and ZnT8. These become autoantibodies - the fingerprints of type 1 diabetes.
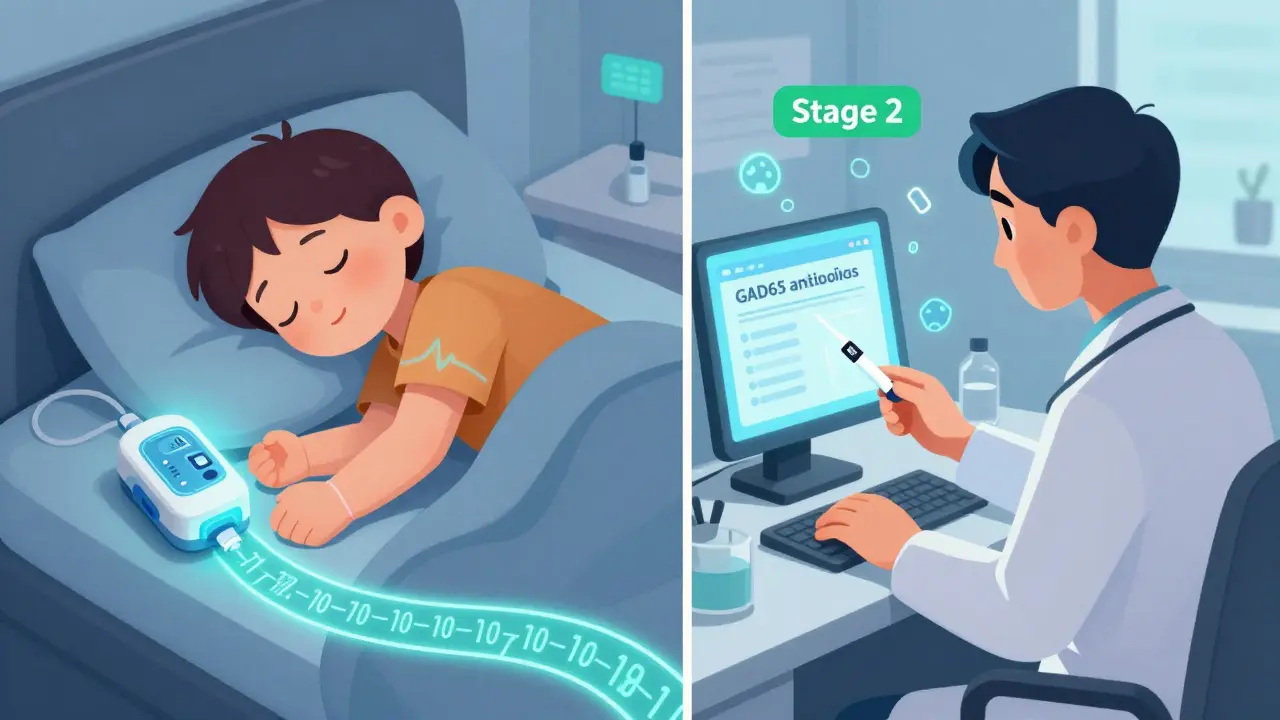
This process doesn’t happen overnight. It can start years before symptoms show. The TrialNet consortium broke it into three stages. Stage 1: you have two or more autoantibodies but normal blood sugar. Stage 2: blood sugar starts rising, but you still feel fine. Stage 3: you’re sick, thirsty, losing weight - and now you need insulin. About 0.4% of the general population is in Stage 1. Only 0.15% make it to Stage 2. But if you’re in Stage 2, you’re almost guaranteed to reach Stage 3 unless something stops it.
Genetics play a big role. If you carry the HLA-DR3/DR4 gene combo, your risk jumps 20 to 30 times higher. But genes alone don’t cause it. Something triggers it. Viruses - especially coxsackievirus B - are the top suspects. Studies show people who test positive for this virus in the months before diagnosis have a 58% higher chance of developing type 1 diabetes. It’s not that the virus causes diabetes. It’s that it wakes up a sleeping autoimmune response in someone already genetically wired for it.
Not everyone with type 1 diabetes is the same. Kids lose their beta cells fast. On average, it takes about 2.8 years from the first autoantibody to full-blown diabetes. Adults? It can take over 12 years. That’s why some adults are misdiagnosed with type 2 diabetes. They’re thin, active, not overweight - but still insulin-dependent. This is called LADA - Latent Autoimmune Diabetes in Adults. About 12% of adults diagnosed with type 2 actually have LADA. And if you don’t know, you get the wrong treatment. Oral meds won’t save you. You’ll burn out what’s left of your pancreas faster.
That’s why testing for autoantibodies matters. If you’re an adult diagnosed with type 2 but you’re not responding to metformin, have no signs of insulin resistance, and are losing weight - get tested. A simple blood test for GAD65 or IA-2 antibodies can change everything. Starting insulin early protects what’s left of your pancreas and prevents dangerous complications.
Insulin is the foundation. But it’s not the whole picture. The American Diabetes Association recommends multiple daily injections (MDI) or an insulin pump. Most people use rapid-acting insulin like aspart or lispro before meals, plus a long-acting basal insulin like glargine U-300 to cover background needs. The starting dose? About 0.5 units per kilogram of body weight per day - split evenly between basal and bolus.
But insulin dosing isn’t guesswork anymore. Continuous glucose monitors (CGMs) like the Dexcom G7 give you real-time data - not just a snapshot, but a movie of your blood sugar. Studies show people using CGMs drop their HbA1c by 0.4 to 0.6% and have 40-50% fewer low blood sugar events. That’s huge. Hypoglycemia isn’t just scary - it’s dangerous. It can cause seizures, accidents, even sudden death.
Even better? Closed-loop systems - the "artificial pancreas." Devices like Tandem’s Control-IQ automatically adjust insulin based on your glucose trends. In 2022, users spent 71-74% of their time in the target range (70-180 mg/dL). People on traditional pumps? Only 51-55%. That’s not a small improvement. That’s life-changing. For parents of kids with type 1, it means fewer night-time alarms, less anxiety, and more sleep.
Here’s something most people don’t know: type 1 diabetes can sometimes show up with another autoimmune condition - autoimmune pancreatitis (AIP). It’s rare - about 1 in 300 cases - but it happens. AIP attacks the exocrine pancreas, the part that makes digestive enzymes. It causes swelling, pain, jaundice, and malabsorption. Unlike type 1, which destroys insulin cells, AIP swells the whole pancreas with immune cells.
There are two types. Type 1 is linked to high IgG4 levels and responds well to steroids. Type 2 is tied to inflammatory bowel disease. When both conditions happen together, it’s a double hit - your insulin production is gone, and your digestion is broken. You need insulin for blood sugar, and pancreatic enzymes for food breakdown. Steroids used to treat AIP can spike blood sugar even more, so insulin doses often need a big jump during treatment.
If you’ve had type 1 for years and suddenly have bloating, greasy stools, or unexplained weight loss, ask your doctor about pancreatic enzyme testing. About 5-10% of long-term type 1 patients develop exocrine insufficiency. It’s not talked about enough - but it’s treatable.
For decades, the goal was just to replace insulin. Now, we’re trying to stop the destruction. In November 2022, the FDA approved teplizumab (Tzield) - the first drug that can delay type 1 diabetes diagnosis. It’s not a cure. But in the PROTECT trial, it pushed back diagnosis by nearly 2.5 years in people with Stage 2 diabetes. That’s two and a half years of normal blood sugar, no insulin, no finger pricks.
It works by calming the T-cells that attack beta cells. It’s given as a 14-day IV infusion. It’s not for everyone - only those with two or more autoantibodies and rising blood sugar. But for families with a child who tests positive, it’s a game-changer.
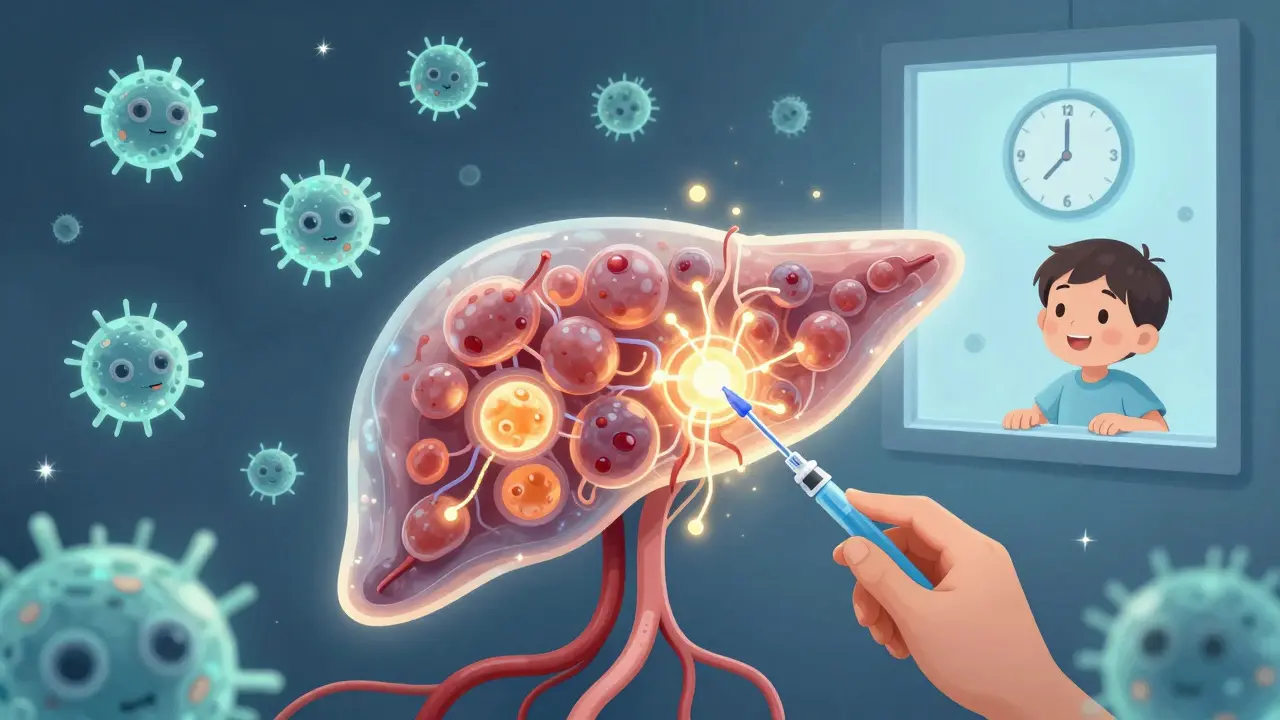
Other drugs are coming. Abatacept, a drug used for rheumatoid arthritis, slowed beta cell loss by 59% in recent-onset type 1 patients. Verapamil, a common blood pressure pill, showed it could preserve 30% more insulin production after a year. And then there’s Vertex’s VX-880 - stem cell-derived islets injected into the liver. In a 2023 trial, 89% of 12 patients became insulin-free for at least 90 days. One patient stayed off insulin for over a year.
This isn’t science fiction. It’s happening now. The future of type 1 diabetes isn’t just better insulin. It’s stopping the immune attack, protecting what’s left of the pancreas, and replacing what’s gone.
If you or someone you love has type 1 diabetes, here’s what matters most:
Type 1 diabetes is not a death sentence. It’s not a life of constant fear. It’s a condition that’s evolving - faster than most people realize. With the right tools, support, and awareness, you can live well. Not just survive. Live well.
No. Type 1 diabetes is an autoimmune disease where the body attacks its own insulin-producing cells. It’s not linked to diet, weight, or lifestyle. While sugar doesn’t cause it, managing blood sugar after diagnosis requires careful attention to carbohydrates - not because sugar caused the disease, but because insulin needs to match food intake.
Currently, there’s no cure. But new therapies like teplizumab can delay diagnosis by years in high-risk people. Stem cell therapies have restored insulin production in some patients, and some have remained insulin-free for over a year. These aren’t widely available yet, but they prove the disease can be modified - not just managed.
Many adults with type 1 diabetes - especially those with slow-progressing LADA - look like type 2 patients: they’re not overweight, they’re active, and they don’t have a family history of type 2. Doctors often assume insulin resistance. But if they’re not responding to oral meds and have autoantibodies, they likely have type 1. Testing for GAD65 or IA-2 antibodies can prevent years of wrong treatment.
When your pancreas makes insulin, it also releases C-peptide in equal amounts. Measuring C-peptide tells you how much insulin your body is still producing - not how much you injected. Low C-peptide means your pancreas is nearly out of insulin-making capacity. High C-peptide means you’re still making some, even if your blood sugar is high. It’s the best way to tell type 1 from type 2.
No. You don’t need to avoid carbs. You need to match your insulin to them. The goal isn’t to eat less carbs - it’s to learn how much insulin you need for each gram of carbohydrate. Many people with type 1 eat high-carb diets successfully using pumps or CGMs. The key is consistency and matching insulin to intake, not restriction.
Absolutely. People with type 1 diabetes compete in the Olympics, raise families, run businesses, and live into their 80s and 90s. The tools today - CGMs, pumps, automated systems - make it safer and easier than ever. The biggest barrier isn’t the disease. It’s outdated myths and lack of access to modern care.
8 Responses
This is the most comprehensive, compassionate breakdown of type 1 I've ever read. Thank you for explaining the autoimmune reality behind the insulin shots. So many people still think it's just 'bad eating habits' - this needs to be shared everywhere.
They're lying to us. The CDC and Big Pharma don't want you to know that glyphosate in your food is what's triggering the autoimmune attack on your pancreas. Look at the spike in cases since 1995 - right after GMOs and Roundup became mainstream. They're selling insulin because they profit from your suffering. C-peptide tests? Just a distraction. The real cure is organic food and detoxing your liver.
Honestly, I find it frustrating that people still treat type 1 like it's some mysterious tragedy. It's a well-documented autoimmune condition with clear biomarkers. If you're an adult diagnosed with 'type 2' and you're not insulin resistant, you're doing yourself a disservice by not getting autoantibody tested. It's not complicated - it's just poorly taught in med school. And yes, LADA is real. I know three people who were misdiagnosed for years.
The statistical breakdown of Stage 1 to Stage 3 progression is accurate, but the article underestimates the role of vitamin D deficiency as a cofactor in autoimmunity. Multiple peer-reviewed studies show serum 25(OH)D levels below 30 ng/mL correlate with increased risk of seroconversion. The TrialNet cohort data doesn't account for this variable. Also, the claim about coxsackievirus B having a 58% increased risk is misleading - it's a relative risk increase from a baseline of 0.02%, making the absolute risk still negligible for most. Correlation ≠ causation.
So let me get this straight - you're telling me I have to spend $1,000 a month on a CGM and a pump just to not die? And the government won't cover it because I'm 'not disabled enough'? Thanks for the pep talk, doc.
The emergence of disease-modifying therapies like teplizumab and VX-880 isn't just a medical breakthrough - it's a paradigm shift. For the first time, we're moving from managing symptoms to altering disease trajectory. The fact that stem cell-derived islets can restore insulin production in humans? That's not sci-fi. That's the new baseline. We're witnessing the birth of a new era in autoimmune medicine, and it's happening faster than most realize. The future isn't just about better insulin - it's about restoring function.
You people are so naive. You think insulin is the problem? Nah. It's the government's secret vaccine program. They put nanoparticles in the flu shots to trigger autoimmunity. Look at the autism rates - same timeline. You think your kid got type 1 because of a virus? Nah. It's because you let them get the MMR at 12 months. I tested my kid's blood - 4 autoantibodies. I refused insulin. Gave him turmeric and colloidal silver. His sugars are fine now. You're all being manipulated.
i read this whole thing and all i got was that if u dont have a pump and a cgm u r basically just waitin 2 die. like bro. its 2024. if u cant afford tech that keeps u alive, that's a system failure. not a personal failure. stop actin like its some miracle cure when it's just basic healthcare. also who the hell is gonna pay for stem cell islet transplants? this is all just rich people medicine with a fancy name.