
Reading a liquid prescription label might seem simple-until you realize your kitchen spoon doesn’t match what the doctor meant. Every year, over 1.3 million people in the U.S. are injured because someone gave the wrong dose of liquid medicine. Most of these errors happen because people misread the label. The good news? It’s not your fault. The system used to be confusing. But now, there are clear rules-and if you know what to look for, you can avoid mistakes.
Every liquid medicine label has three critical pieces of information. If you miss any one of them, you could give too much-or too little.
People often mix up concentration and total volume. If you see “500 mL” on the bottle, that doesn’t mean take 500 mL. That’s just how big the bottle is. The dose is always based on the concentration.
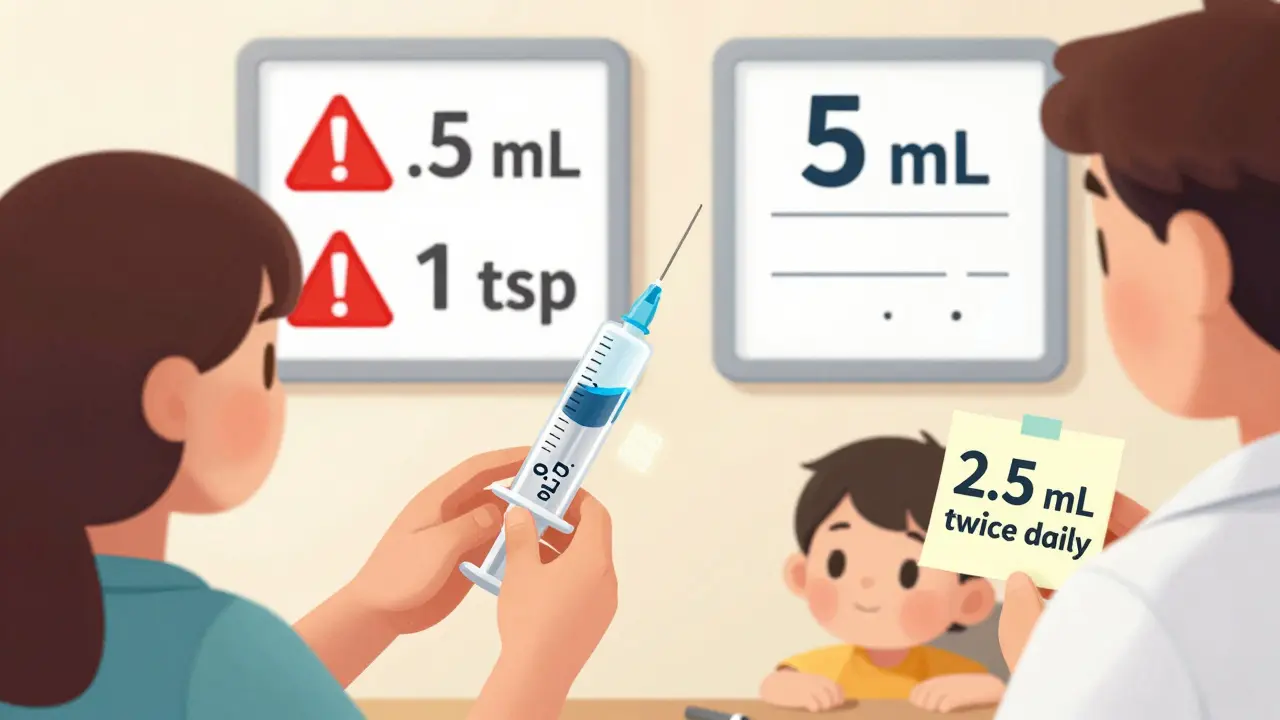
Old labels used teaspoons and tablespoons. That’s dangerous. A household teaspoon can hold anywhere from 2.5 mL to 7.5 mL. A tablespoon? It might be 5 mL-or it might be 20 mL. That’s a 300% difference. The FDA and the National Council for Prescription Drug Programs (NCPDP) banned those units on prescriptions in 2016. Now, every label must use milliliters (mL) only.
Here’s what you need to know about how mL is written:
These rules aren’t suggestions. They’re backed by research. A Johns Hopkins study found that following these formatting rules cuts 10-fold dosing errors by 47%.
Never use a kitchen spoon. Always use the measuring device that came with the medicine. It might be a syringe, a cup, or a dropper. But even those can be misleading.
Check the markings on the device. Some only show mL. Others show both mL and teaspoons. If it shows teaspoons, ignore them. Rely only on the mL numbers. The FDA says that’s the only safe way.
Here’s what to look for:
Some devices measure as little as 0.001 mL. Others max out at 5 mL. If your dose is 7.5 mL and the device only goes to 5 mL, you’ll need to give two doses. Don’t guess. Ask the pharmacist to show you how.
Even with standardization, mistakes still happen. In a 2021 study, 17.3% of negative pharmacy reviews mentioned confusion over liquid doses. The most common mistake? Misreading the concentration.
Example: The label says 160 mg per 5 mL. You’re told to give 10 mL. That’s correct-it’s two doses of 5 mL. But if you think the 160 mg is the total dose, you might only give 5 mL and under-medicate.
Here’s what to do if you’re unsure:
Studies show that using teach-back reduces dosing errors by 63%. It’s not about being “stupid.” It’s about making sure the information stuck.
Only 12% of U.S. adults have proficient health literacy, according to the National Assessment of Adult Literacy. That means most people struggle with basic medical terms-even if the label is perfectly clear.
Here’s what you can do:
Parents who get a live demonstration from a pharmacist are 78% less likely to make a mistake. That’s huge. Don’t be shy-ask for help. Pharmacists are trained for this.
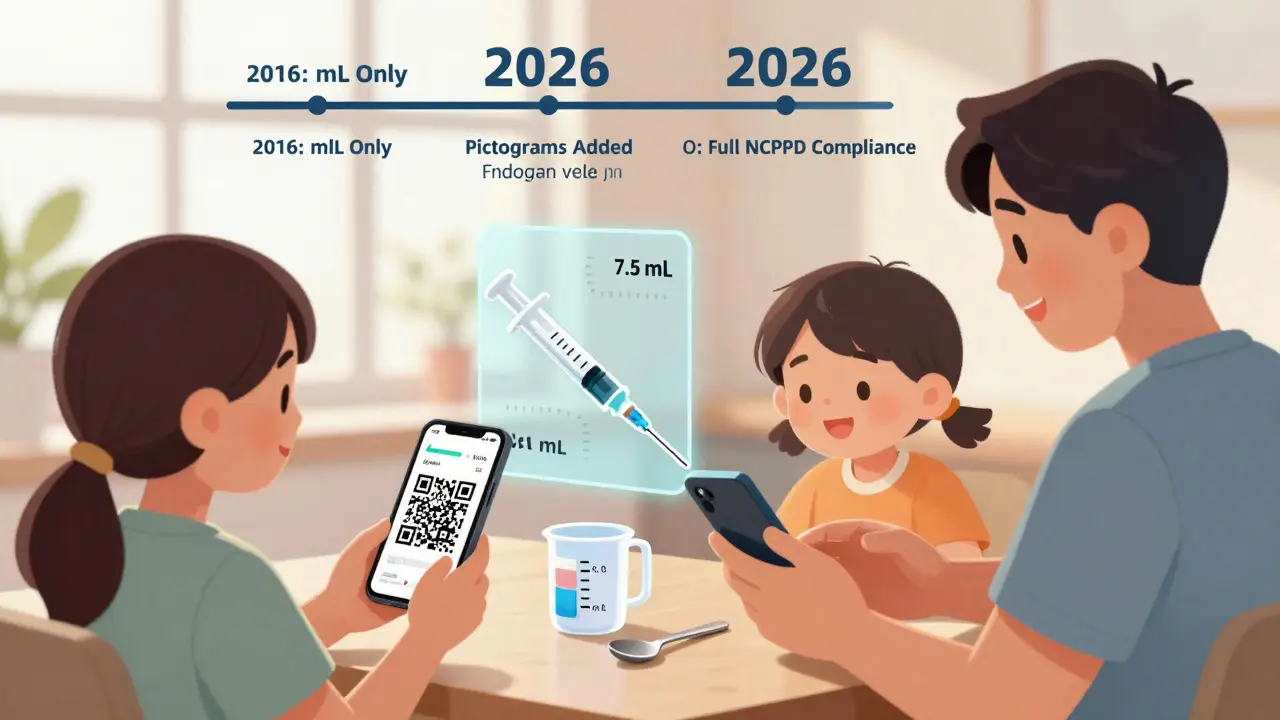
The rules are getting stricter. In 2023, the FDA proposed new rules requiring pictograms on liquid labels-simple pictures showing how to fill the syringe or cup. Early tests showed a 37% drop in errors when families used these visuals.
Some pharmacies, like Amazon Pharmacy and Medly, now include QR codes on labels. Scan it, and a short video shows you exactly how to measure the dose. That’s becoming the new standard.
By 2026, experts predict nearly all pharmacies will follow the NCPDP standards fully. But until then, you still need to be the final safety check.
Medication errors are preventable. You don’t need to be a doctor. You just need to know what to look for-and when to ask.
It means every 5 milliliters of the liquid contains 240 milligrams of the active drug. If your dose is 120 mg, you need to give half of that volume: 2.5 mL. Always calculate the dose based on the concentration, not the total bottle size.
No. Household teaspoons vary from 2.5 mL to 7.5 mL. That’s a 200% difference. Even a small error can lead to under-dosing or dangerous overdose. Always use the measuring device that came with the medicine.
The correct format is '0.5 mL.' The leading zero prevents misreading it as '5 mL,' which could cause a 10-fold overdose. The FDA and NCPDP require this format. If you see '.5 mL,' it’s outdated and potentially dangerous.
If your dose is 3.7 mL but the syringe only marks 3 mL and 4 mL, ask the pharmacist for a more precise device. Some syringes measure to 0.1 mL. Never guess. You can also ask if the dose can be adjusted to match what’s available.
No. Liquid medicines lose potency after expiration and can grow harmful bacteria. Even if it looks fine, throw it out. The concentration may no longer be accurate, which makes dosing unsafe.
Some independent pharmacies haven’t updated their old systems. But by law, the dose must be written in mL. If you see teaspoons, ask the pharmacist to re-label it in mL. You have the right to safe, standardized instructions.
Signs of overdose include drowsiness, vomiting, or trouble breathing. Signs of under-dosing include no improvement in symptoms after 48 hours. If you’re unsure, call your doctor or pharmacist. Never adjust the dose without professional advice.
Yes. Some pharmacies offer QR codes on labels that link to video instructions. Apps like Medisafe and MyTherapy can track doses and remind you when to give medicine. But always verify the dose with the physical label and measuring device first.
Right now, find a bottle of liquid medicine in your home. Look at the label. Can you explain the concentration? Can you point to the dose on the measuring device? If not, call the pharmacy. Ask them to walk you through it. Do it before the next dose is due.
Medication safety isn’t about memorizing rules. It’s about asking questions. It’s about double-checking. And it’s about never assuming-especially when it’s your child’s health on the line.
9 Responses
This whole post is just corporate propaganda dressed up as public service. They banned teaspoons? Big deal. The real problem is that pharma companies still design labels like they’re trying to confuse people on purpose. I’ve seen bottles where the concentration is printed in 6-point font next to a giant ‘300 mL’-like, who’s the target audience here, lawyers? And don’t even get me started on QR codes. Next they’ll be requiring a VPN to read a medicine label.
Thank you for this incredibly important guide 🙏 I’m a mom of two and I had no idea about the leading zero rule-so glad I learned this before giving my son his antibiotics. I’ve started writing the dose on a sticky note and keeping it next to the syringe. It’s made me feel so much more confident. Please keep sharing this kind of info-it saves lives 💕
Look, I’m not a doctor but I’ve read a lot of medical blogs and this is just common sense. You don’t use a spoon. You use the thing that comes with it. Why is this even a thing? People are stupid. And the FDA had to ban teaspoons? That’s like banning knives because someone cut their finger. This post is just proof that we’ve turned parenting into a compliance test. Also, 0.5 mL? That’s half a drop. Who measures that? You need a microscope. I just eyeball it. My kid’s fine.
OMG I just read this and immediately checked my daughter’s cough syrup bottle 🥲 I was using the cap because it had markings-I had NO IDEA they were misleading! I’m calling the pharmacy right now to ask for a new syringe. Also, the teach-back thing? That’s genius. I’m going to start doing that with my sister who helps with the kids. You’re right-this isn’t about being smart, it’s about being safe. Thank you for writing this. ❤️
While I appreciate the effort behind this guide, it’s clear that the underlying issue is systemic failure. The FDA’s ‘standardization’ is a performative gesture. Real reform would require dismantling the profit-driven pharmacy model that incentivizes complexity. Why do you think QR codes are being pushed? Because they shift liability onto the consumer. ‘Scan this video’-sure, if you have Wi-Fi, a smartphone, and the cognitive bandwidth to parse corporate UX. Meanwhile, elderly patients and low-income families are left holding a syringe with no context. This isn’t safety-it’s surveillance capitalism with a pediatric twist.
Wow. Just wow. You spent 2,000 words telling people not to use spoons? Newsflash: people are dumb. That’s not a design flaw-that’s a biological reality. And now you’re telling them to ‘ask the pharmacist’? Most pharmacists are overworked, underpaid, and can’t even spell ‘milliliter’ on a bad day. This whole thing is a feel-good distraction. The real solution? Stop giving liquid meds to kids. Give them pills. Or better yet-stop prescribing so much medicine in the first place. This post is a luxury for people who think healthcare is a puzzle to solve, not a system designed to fail them.
I used to give my son medicine with a spoon until I read this. Now I use the syringe and write the dose down. It’s so much easier. I wish I’d known this sooner. Thanks for making it simple.
bro why you even using liquid medicine? just give them pill. i live in india, we use tablets for everything. even kids. no mess. no measuring. no stress. why america so complicated? also why you need qr code to read a bottle? it's 2025, not 1995.
Let’s be honest-this isn’t about dosing. It’s about control. The system wants you dependent on devices, QR codes, and pharmacists because if you could just read a label and trust yourself, you’d stop taking so much medicine. They’ve turned parenting into a compliance nightmare. And now you’re supposed to be grateful because they stopped using teaspoons? Please. The real crime is that we’ve been trained to believe that health is something you buy, measure, and scan-not something you understand. You didn’t solve the problem. You just made it look prettier.